Abstract
Technologies for imaging the pathophysiology of Alzheimer disease (AD) now permit studies of the relationships between the two major proteins deposited in this disease — amyloid-β (Aβ) and tau — and their effects on measures of neurodegeneration and cognition in humans. Deposition of Aβ in the medial parietal cortex appears to be the first stage in the development of AD, although tau aggregates in the medial temporal lobe (MTL) precede Aβ deposition in cognitively healthy older people. Whether aggregation of tau in the MTL is the first stage in AD or a fairly benign phenomenon that may be transformed and spread in the presence of Aβ is a major unresolved question. Despite a strong link between Aβ and tau, the relationship between Aβ and neurodegeneration is weak; rather, it is tau that is associated with brain atrophy and hypometabolism, which, in turn, are related to cognition. Although there is support for an interaction between Aβ and tau resulting in neurodegeneration that leads to dementia, the unknown nature of this interaction, the strikingly different patterns of brain Aβ and tau deposition and the appearance of neurodegeneration in the absence of Aβ and tau are challenges to this model that ultimately must be explained.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Small, S. A., Schobel, S. A., Buxton, R. B., Witter, M. P. & Barnes, C. A. A pathophysiological framework of hippocampal dysfunction in ageing and disease. Nat. Rev. Neurosci. 12, 585–601 (2011).
Nelson, P. T. et al. Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J. Neuropathol. Exp. Neurol. 71, 362–381 (2012).
Ittner, L. M. & Gotz, J. Amyloid-β and tau — a toxic pas de deux in Alzheimer’s disease. Nat. Rev. Neurosci. 12, 65–72 (2011).
Hyman, B. T. et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 8, 1–13 (2012).
Price, J. L. & Morris, J. C. Tangles and plaques in nondemented aging and “preclinical” Alzheimer’s disease. Ann. Neurol. 45, 358–368 (1999).
Bennett, D. A. et al. Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology 66, 1837–1844 (2006).
Jack, C. R. Jr. et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12, 207–216 (2013). This paper proposes a model of the pathophysiology of AD that has been influential in guiding and interpreting human studies.
Hardy, J. & Selkoe, D. J. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297, 353–356 (2002).
Wingo, T. S., Lah, J. J., Levey, A. I. & Cutler, D. J. Autosomal recessive causes likely in early-onset Alzheimer disease. Arch. Neurol. 69, 59–64 (2012).
Cacace, R., Sleegers, K. & Van Broeckhoven, C. Molecular genetics of early-onset Alzheimer’s disease revisited. Alzheimers Dement. 12, 733–748 (2016).
Josephs, K. A. et al. Rates of hippocampal atrophy and presence of post-mortem TDP-43 in patients with Alzheimer’s disease: a longitudinal retrospective study. Lancet Neurol. 16, 917–924 (2017).
Schneider, J. A., Arvanitakis, Z., Leurgans, S. E. & Bennett, D. A. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann. Neurol. 66, 200–208 (2009).
Bertram, L., Lill, C. M. & Tanzi, R. E. The genetics of Alzheimer disease: back to the future. Neuron 68, 270–281 (2010).
Lopera, F. et al. Clinical features of early-onset Alzheimer disease in a large kindred with an E280A presenilin-1 mutation. JAMA 277, 793–799 (1997).
Buckner, R. L. et al. Molecular, structural, and functional characterization of Alzheimer’s disease: evidence for a relationship between default activity, amyloid, and memory. J. Neurosci. 25, 7709–7717 (2005).
Grothe, M. J., Teipel, S. J. & Alzheimer’s Disease Neuroimaging Initiative. Spatial patterns of atrophy, hypometabolism, and amyloid deposition in Alzheimer’s disease correspond to dissociable functional brain networks. Hum. Brain Mapp. 37, 35–53 (2016).
Buckner, R. L. et al. Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer’s disease. J. Neurosci. 29, 1860–1873 (2009).
Daianu, M. et al. Rich club analysis in the Alzheimer’s disease connectome reveals a relatively undisturbed structural core network. Hum. Brain Mapp. 36, 3087–3103 (2015).
Fox, N. C. et al. Presymptomatic hippocampal atrophy in Alzheimer’s disease. A longitudinal MRI study. Brain 119, 2001–2007 (1996).
Scholl, M. et al. Low PiB PET retention in presence of pathologic CSF biomarkers in Arctic APP mutation carriers. Neurology 79, 229–236 (2012).
Bateman, R. J. et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N. Engl. J. Med. 367, 795–804 (2012). This article is an examination of the sequence of pathophysiological events in the presymptomatic phase of ADAD.
Fleisher, A. S. et al. Florbetapir PET analysis of amyloid-β deposition in the presenilin 1 E280A autosomal dominant Alzheimer’s disease kindred: a cross-sectional study. Lancet Neurol. 11, 1057–1065 (2012).
Benzinger, T. L. et al. Regional variability of imaging biomarkers in autosomal dominant Alzheimer’s disease. Proc. Natl Acad. Sci. USA 110, E4502–E4509 (2013).
Fleisher, A. S. et al. Associations between biomarkers and age in the presenilin 1 E280A autosomal dominant Alzheimer disease kindred: a cross-sectional study. JAMA Neurol. 72, 316–324 (2015).
Chhatwal, J. P. et al. Impaired default network functional connectivity in autosomal dominant Alzheimer disease. Neurology 81, 736–744 (2013).
Klunk, W. E. et al. Amyloid deposition begins in the striatum of presenilin-1 mutation carriers from two unrelated pedigrees. J. Neurosci. 27, 6174–6184 (2007).
Villemagne, V. L. et al. High striatal amyloid β-peptide deposition across different autosomal Alzheimer disease mutation types. Arch. Neurol. 66, 1537–1544 (2009).
Gordon, B. A. et al. Spatial patterns of neuroimaging biomarker change in individuals from families with autosomal dominant Alzheimer’s disease: a longitudinal study. Lancet Neurol. 17, 241–250 (2018).
Quiroz, Y. T. et al. Association between amyloid and tau accumulation in young adults with autosomal dominant Alzheimer disease. JAMA Neurol. 75, 548–556 (2018).
Gorno-Tempini, M. L. et al. Classification of primary progressive aphasia and its variants. Neurology 76, 1006–1014 (2011).
Mendez, M. F., Ghajarania, M. & Perryman, K. M. Posterior cortical atrophy: clinical characteristics and differences compared to Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 14, 33–40 (2002).
Ossenkoppele, R. et al. The behavioural/dysexecutive variant of Alzheimer’s disease: clinical, neuroimaging and pathological features. Brain 138, 2732–2749 (2015).
Rabinovici, G. D. et al. Aβ amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann. Neurol. 64, 388–401 (2008).
de Souza, L. C. et al. Similar amyloid-β burden in posterior cortical atrophy and Alzheimer’s disease. Brain 134, 2036–2043 (2011).
Lehmann, M. et al. Diverging patterns of amyloid deposition and hypometabolism in clinical variants of probable Alzheimer’s disease. Brain 136, 844–858 (2013).
Ossenkoppele, R. et al. Tau PET patterns mirror clinical and neuroanatomical variability in Alzheimer’s disease. Brain 139, 1551–1567 (2016). This report shows the strong relationships between tau, glucose metabolism and cognitive phenotype in EOAD.
Mielke, R., Herholz, K., Grond, M., Kessler, J. & Heiss, W. D. Differences of regional cerebral glucose metabolism between presenile and senile dementia of Alzheimer type. Neurobiol. Aging 13, 93–98 (1992).
Kim, E. J. et al. Glucose metabolism in early onset versus late onset Alzheimer’s disease: an SPM analysis of 120 patients. Brain 128, 1790–1801 (2005).
Rabinovici, G. D. et al. Increased metabolic vulnerability in early-onset Alzheimer’s disease is not related to amyloid burden. Brain 133, 512–528 (2010).
Xia, C. et al. Association of in vivo [18F]AV-1451 tau PET imaging results with cortical atrophy and symptoms in typical and atypical Alzheimer disease. JAMA Neurol. 74, 427–436 (2017).
Schöll, M. et al. Distinct 18F-AV-1451 tau PET retention patterns in early- and late-onset Alzheimer’s disease. Brain 140, 2286–2294 (2017).
Bejanin, A. et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer’s disease. Brain 140, 3286–3300 (2017).
Iaccarino, L. et al. Local and distant relationships between amyloid, tau and neurodegeneration in Alzheimer’s disease. Neuroimage Clin. 17, 452–464 (2018).
Whitwell, J. L. et al. [18F]AV-1451 clustering of entorhinal and cortical uptake in Alzheimer’s disease. Ann. Neurol. 83, 248–257 (2018).
Klunk, W. E. et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh compound-B. Ann. Neurol. 55, 306–319 (2004). This article presents the initial report of the use of amyloid imaging in the study of ageing and dementia.
Rowe, C. C. et al. Imaging β-amyloid burden in aging and dementia. Neurology 68, 1718–1725 (2007).
Furst, A. J. et al. Cognition, glucose metabolism and amyloid burden in Alzheimer’s disease. Neurobiol. Aging 33, 215–225 (2012).
Singh, V. et al. Spatial patterns of cortical thinning in mild cognitive impairment and Alzheimer’s disease. Brain 129, 2885–2893 (2006).
Dickerson, B. C. et al. The cortical signature of Alzheimer’s disease: regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cereb. Cortex 19, 497–510 (2009). This paper reports on the use of MRI to identify a characteristic pattern of regional brain atrophy associated with AD and in asymptomatic older people.
Whitwell, J. L. et al. 3D maps from multiple MRI illustrate changing atrophy patterns as subjects progress from mild cognitive impairment to Alzheimer’s disease. Brain 130, 1777–1786 (2007).
Silverman, D. H. et al. Positron emission tomography in evaluation of dementia: regional brain metabolism and long-term outcome. JAMA 286, 2120–2127 (2001).
Fouquet, M. et al. Longitudinal brain metabolic changes from amnestic mild cognitive impairment to Alzheimer’s disease. Brain 132, 2058–2067 (2009).
Landau, S. M. et al. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiol. Aging 32, 1207–1218 (2011).
De Santi, S. et al. Hippocampal formation glucose metabolism and volume losses in MCI and AD. Neurobiol. Aging 22, 529–539 (2001).
Jack, C. R. Jr. et al. Comparison of different MRI brain atrophy rate measures with clinical disease progression in AD. Neurology 62, 591–600 (2004).
Jack, C. R. Jr. et al. Brain β-amyloid measures and magnetic resonance imaging atrophy both predict time-to-progression from mild cognitive impairment to Alzheimer’s disease. Brain 133, 3336–3348 (2010).
Chetelat, G. et al. Relationship between atrophy and β-amyloid deposition in Alzheimer disease. Ann. Neurol. 67, 317–324 (2010).
Ewers, M. et al. CSF biomarker and PIB-PET-derived β-amyloid signature predicts metabolic, gray matter, and cognitive changes in nondemented subjects. Cereb. Cortex 22, 1993–2004 (2012).
Tosun, D. et al. Spatial patterns of brain amyloid-β burden and atrophy rate associations in mild cognitive impairment. Brain 134, 1077–1088 (2011).
Archer, H. A. et al. Amyloid load and cerebral atrophy in Alzheimer’s disease: an 11C-PIB positron emission tomography study. Ann. Neurol. 60, 145–147 (2006).
Greicius, M. D., Srivastava, G., Reiss, A. L. & Menon, V. Default-mode network activity distinguishes Alzheimer’s disease from healthy aging: evidence from functional MRI. Proc. Natl Acad. Sci. USA 101, 4637–4642 (2004). This paper presents the initial report showing the effects of AD on resting-state connectivity in the DMN.
Badhwar, A. et al. Resting-state network dysfunction in Alzheimer’s disease: a systematic review and meta-analysis. Alzheimers Dement. 8, 73–85 (2017).
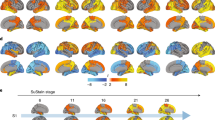
Braak, H. & Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 82, 239–259 (1991). This landmark report describes the results of autopsy studies of AD pathology that proposed a widely utilized staging scheme for tau pathology.
Schwarz, A. J. et al. Regional profiles of the candidate tau PET ligand 18F-AV-1451 recapitulate key features of Braak histopathological stages. Brain 139, 1539–1550 (2016).
Johnson, K. A. et al. Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann. Neurol. 79, 110–119 (2016). This report examines the use of tau-PET in individuals ranging from those who were cognitively healthy to those with dementia.
Cho, H. et al. In vivo cortical spreading pattern of tau and amyloid in the Alzheimer disease spectrum. Ann. Neurol. 80, 247–258 (2016).
Brier, M. R. et al. Tau and Aβ imaging, CSF measures, and cognition in Alzheimer’s disease. Sci. Transl Med. 8, 338ra66 (2016).
Pontecorvo, M. J. et al. Relationships between flortaucipir PET tau binding and amyloid burden, clinical diagnosis, age and cognition. Brain 140, 748–763 (2017).
Wang, L. et al. Evaluation of tau imaging in staging Alzheimer disease and revealing interactions between β-amyloid and tauopathy. JAMA Neurol. 73, 1070–1077 (2016).
Hansson, O. et al. Tau pathology distribution in Alzheimer’s disease corresponds differentially to cognition-relevant functional brain networks. Front. Neurosci. 11, 167 (2017).
Hoenig, M. C. et al. Networks of tau distribution in Alzheimer’s disease. Brain 141, 568–581 (2018).
Bischof, G. N. et al. Impact of tau and amyloid burden on glucose metabolism in Alzheimer’s disease. Ann. Clin. Transl Neurol. 3, 934–939 (2016).
Jansen, W. J. et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA 313, 1924–1938 (2015).
Morris, J. C. et al. APOE predicts amyloid-β but not tau Alzheimer pathology in cognitively normal aging. Ann. Neurol. 67, 122–131 (2010).
Farrer, L. A. et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278, 1349–1356 (1997).
Villeneuve, S. et al. Existing Pittsburgh compound-B positron emission tomography thresholds are too high: statistical and pathological evaluation. Brain 138, 2020–2033 (2015).
Palmqvist, S. et al. Earliest accumulation of β-amyloid occurs within the default-mode network and concurrently affects brain connectivity. Nat. Commun. 8, 1214 (2017).
Hedden, T., Oh, H., Younger, A. P. & Patel, T. A. Meta-analysis of amyloid-cognition relations in cognitively normal older adults. Neurology 80, 1341–1348 (2013).
Jansen, W. J. et al. Association of cerebral amyloid-β aggregation with cognitive functioning in persons without dementia. JAMA Psychiatry 75, 84–95 (2018).
Donohue, M. C. et al. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA 317, 2305–2316 (2017). This large multisite study analyses the relationship between Aβ and cognitive decline in healthy older people.
Dubois, B. et al. Cognitive and neuroimaging features and brain β-amyloidosis in individuals at risk of Alzheimer’s disease (INSIGHT-preAD): a longitudinal observational study. Lancet Neurol. 17, 335–346 (2018).
Mormino, E. C. et al. Amyloid and APOE ε4 interact to influence short-term decline in preclinical Alzheimer disease. Neurology 82, 1760–1767 (2014).
Farrell, M. E. et al. Association of longitudinal cognitive decline with amyloid burden in middle-aged and older adults: evidence for a dose-response relationship. JAMA Neurol. 74, 830–838 (2017).
Becker, J. A. et al. Amyloid-β associated cortical thinning in clinically normal elderly. Ann. Neurol. 69, 1032–1042 (2011).
Chetelat, G. et al. Accelerated cortical atrophy in cognitively normal elderly with high β-amyloid deposition. Neurology 78, 477–484 (2012).
Dore, V. et al. Cross-sectional and longitudinal analysis of the relationship between Aβ deposition, cortical thickness, and memory in cognitively unimpaired individuals and in Alzheimer disease. JAMA Neurol. 70, 903–911 (2013).
Villemagne, V. L. et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 12, 357–367 (2013).
Lowe, V. J. et al. Association of hypometabolism and amyloid levels in aging, normal subjects. Neurology 82, 1959–1967 (2014).
Reiman, E. M. et al. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer’s dementia. Proc. Natl Acad. Sci. USA 101, 284–289 (2004).
Jagust, W. J. & Landau, S. M. & Alzheimer’s Disease Neuroimaging Initiative. Apolipoprotein E, not fibrillar β-amyloid, reduces cerebral glucose metabolism in normal aging. J. Neurosci. 32, 18227–18233 (2012).
Altmann, A. et al. Regional brain hypometabolism is unrelated to regional amyloid plaque burden. Brain 138, 3734–3746 (2015).
Cohen, A. D. et al. Basal cerebral metabolism may modulate the cognitive effects of Aβ in mild cognitive impairment: an example of brain reserve. J. Neurosci. 29, 14770–14778 (2009).
Johnson, S. C. et al. Amyloid burden and neural function in people at risk for Alzheimer’s disease. Neurobiol. Aging 35, 576–584 (2014).
Oh, H., Madison, C., Baker, S., Rabinovici, G. & Jagust, W. Dynamic relationships between age, amyloid-β deposition, and glucose metabolism link to the regional vulnerability to Alzheimer’s disease. Brain 139, 2275–2289 (2016).
Hedden, T. et al. Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J. Neurosci. 29, 12686–12694 (2009).
Mormino, E. C. et al. Relationships between β-amyloid and functional connectivity in different components of the default mode network in aging. Cereb. Cortex 21, 2399–2407 (2011).
Jones, D. T. et al. Cascading network failure across the Alzheimer’s disease spectrum. Brain 139, 547–562 (2016).
Mormino, E. C. et al. Aβ deposition in aging is associated with increases in brain activation during successful memory encoding. Cereb. Cortex 22, 1813–1823 (2012).
Sperling, R. A. et al. Amyloid deposition is associated with impaired default network function in older persons without dementia. Neuron 63, 178–188 (2009).
Kennedy, K. M. et al. Effects of β-amyloid accumulation on neural function during encoding across the adult lifespan. Neuroimage 62, 1–8 (2012).
Schöll, M. et al. PET imaging of tau deposition in the aging human brain. Neuron 89, 971–982 (2016).
Braak, H. & Del Tredici, K. Where, when, and in what form does sporadic Alzheimer’s disease begin? Curr. Opin. Neurol. 25, 708–714 (2012).
Tosun, D. et al. Association between tau deposition and antecedent amyloid-β accumulation rates in normal and early symptomatic individuals. Brain 140, 1499–1512 (2017).
Leal, S. L., Lockhart, S. N., Maass, A., Bell, R. K. & Jagust, W. J. Subthreshold amyloid predicts tau deposition in aging. J. Neurosci. 38, 4482–4489 (2018).
Lowe, V. J. et al. Widespread brain tau and its association with ageing, Braak stage and Alzheimer’s dementia. Brain 141, 271–287 (2018).
Jack, C. R. Jr. et al. Longitudinal tau PET in ageing and Alzheimer’s disease. Brain 141, 1517–1528 (2018).
Sepulcre, J. et al. In vivo tau, amyloid, and gray matter profiles in the aging brain. J. Neurosci. 36, 7364–7374 (2016).
Lockhart, S. N. et al. Amyloid and tau PET demonstrate region-specific associations in normal older people. Neuroimage 150, 191–199 (2017).
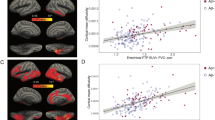
Maass, A. et al. Entorhinal tau pathology, episodic memory decline, and neurodegeneration in aging. J. Neurosci. 38, 530–543 (2018). This paper reports on the structural and cognitive effects of MTL tau deposition in normal ageing.
LaPoint, M. R. et al. The association between tau PET and retrospective cortical thinning in clinically normal elderly. Neuroimage 157, 612–622 (2017).
Hanseeuw, B. J. et al. Fluorodeoxyglucose metabolism associated with tau-amyloid interaction predicts memory decline. Ann. Neurol. 81, 583–596 (2017).
Adams, J. N., Lockhart, S. N., Li, L. & Jagust, W. J. Relationships between tau and glucose metabolism reflect Alzheimer’s disease pathology in cognitively normal older adults. Cereb. Cortex. https://doi.org/10.1093/cercor/bhy078 (2018).
Sepulcre, J. et al. Tau and amyloid β proteins distinctively associate to functional network changes in the aging brain. Alzheimers Dement. 13, 1261–1269 (2017).
Marks, S. M., Lockhart, S. N., Baker, S. L. & Jagust, W. J. Tau and β-amyloid are associated with medial temporal lobe structure, function, and memory encoding in normal aging. J. Neurosci. 37, 3192–3201 (2017).
DeCarli, C. et al. Measures of brain morphology and infarction in the framingham heart study: establishing what is normal. Neurobiol. Aging 26, 491–510 (2005).
Gautam, P., Cherbuin, N., Sachdev, P. S., Wen, W. & Anstey, K. J. Relationships between cognitive function and frontal grey matter volumes and thickness in middle aged and early old-aged adults: the PATH Through Life study. Neuroimage 55, 845–855 (2011).
Zuendorf, G., Kerrouche, N., Herholz, K. & Baron, J. C. Efficient principal component analysis for multivariate 3D voxel-based mapping of brain functional imaging data sets as applied to FDG-PET and normal aging. Hum. Brain Mapp. 18, 13–21 (2003).
Smith, C. D. et al. Brain structural alterations before mild cognitive impairment. Neurology 68, 1268–1273 (2007).
Dickerson, B. C. et al. Alzheimer-signature MRI biomarker predicts AD dementia in cognitively normal adults. Neurology 76, 1395–1402 (2011).
de Leon, M. J. et al. Prediction of cognitive decline in normal elderly subjects with 2-[(18)F]fluoro-2-deoxy-D-glucose/poitron-emission tomography (FDG/PET). Proc. Natl Acad. Sci. USA 98, 10966–10971 (2001).
Jagust, W. et al. Brain imaging evidence of preclinical Alzheimer’s disease in normal aging. Ann. Neurol. 59, 673–681 (2006).
Knopman, D. S. et al. Brain injury biomarkers are not dependent on β-amyloid in normal elderly. Ann. Neurol. 73, 472–480 (2013).
Bakkour, A., Morris, J. C., Wolk, D. A. & Dickerson, B. C. The effects of aging and Alzheimer’s disease on cerebral cortical anatomy: specificity and differential relationships with cognition. Neuroimage 76, 332–344 (2013).
Fjell, A. M. et al. Brain changes in older adults at very low risk for Alzheimer’s disease. J. Neurosci. 33, 8237–8242 (2013).
Jack, C. R. Jr. et al. Suspected non-Alzheimer disease pathophysiology — concept and controversy. Nat. Rev. Neurol. 12, 117–124 (2016). This article reviews the factors that may be associated with neurodegeneration in the absence of AD pathology.
Burnham, S. C. et al. Clinical and cognitive trajectories in cognitively healthy elderly individuals with suspected non-Alzheimer’s disease pathophysiology (SNAP) or Alzheimer’s disease pathology: a longitudinal study. Lancet Neurol. 15, 1044–1053 (2016).
Crary, J. F. et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 128, 755–766 (2014).
Mormino, E. C. et al. Heterogeneity in suspected non-Alzheimer disease pathophysiology among clinically normal older individuals. JAMA Neurol. 73, 1185–1191 (2016).
Jack, C. R. Jr. et al. Age-specific and sex-specific prevalence of cerebral β-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50–95 years: a cross-sectional study. Lancet Neurol. 16, 435–444 (2017).
Brookmeyer, R. & Abdalla, N. Estimation of lifetime risks of Alzheimer’s disease dementia using biomarkers for preclinical disease. Alzheimers Dement. 14, 981–988 (2018).
Caminiti, S. P. et al. FDG-PET and CSF biomarker accuracy in prediction of conversion to different dementias in a large multicentre MCI cohort. Neuroimage Clin. 18, 167–177 (2018).
Lehmann, M. et al. Intrinsic connectivity networks in healthy subjects explain clinical variability in Alzheimer’s disease. Proc. Natl Acad. Sci. USA 110, 11606–11611 (2013).
DeKosky, S. T. & Scheff, S. W. Synapse loss in frontal cortex biopsies in Alzheimer’s disease: correlation with cognitive severity. Ann. Neurol. 27, 457–464 (1990).
Terry, R. D. et al. Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann. Neurol. 30, 572–580 (1991).
Chen, M. K. et al. Assessing synaptic density in Alzheimer disease with synaptic vesicle glycoprotein 2A positron emission tomographic imaging. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2018.1836 (2018).
Kuhl, D. E. et al. In vivo mapping of cerebral acetylcholinesterase activity in aging and Alzheimer’s disease. Neurology 52, 691–699 (1999).
Nitsch, R. M., Farber, S. A., Growdon, J. H. & Wurtman, R. J. Release of amyloid beta-protein precursor derivatives by electrical depolarization of rat hippocampal slices. Proc. Natl Acad. Sci. USA 90, 5191–5193 (1993).
Kamenetz, F. et al. APP processing and synaptic function. Neuron 37, 925–937 (2003).
Cirrito, J. R. et al. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron 48, 913–922 (2005).
Bero, A. W. et al. Neuronal activity regulates the regional vulnerability to amyloid-β deposition. Nat. Neurosci. 14, 750–756 (2011).
Pooler, A. M., Phillips, E. C., Lau, D. H., Noble, W. & Hanger, D. P. Physiological release of endogenous tau is stimulated by neuronal activity. EMBO Rep. 14, 389–394 (2013).
Wu, J. W. et al. Neuronal activity enhances tau propagation and tau pathology in vivo. Nat. Neurosci. 19, 1085–1092 (2016).
Elman, J. A. et al. Effects of beta-amyloid on resting state functional connectivity within and between networks reflect known patterns of regional vulnerability. Cereb. Cortex 26, 695–707 (2016).
Tomasi, D., Wang, G. J. & Volkow, N. D. Energetic cost of brain functional connectivity. Proc. Natl Acad. Sci. USA 110, 13642–13647 (2013).
Grothe, M. J. et al. Molecular properties underlying regional vulnerability to Alzheimer’s disease pathology. Brain 141, 2755–2771 (2018).
Vlassenko, A. G. et al. Spatial correlation between brain aerobic glycolysis and amyloid-β (Aβ) deposition. Proc. Natl Acad. Sci. USA 107, 17763–17767 (2010).
Leal, S. L., Landau, S. M., Bell, R. K. & Jagust, W. J. Hippocampal activation is associated with longitudinal amyloid accumulation and cognitive decline. Elife 8, e22978 (2017).
Schultz, A. P. et al. Phases of hyperconnectivity and hypoconnectivity in the default mode and salience networks track with amyloid and tau in clinically normal individuals. J. Neurosci. 37, 4323–4331 (2017).
Bakker, A. et al. Reduction of hippocampal hyperactivity improves cognition in amnestic mild cognitive impairment. Neuron 74, 467–474 (2012).
Seeley, W. W., Crawford, R. K., Zhou, J., Miller, B. L. & Greicius, M. D. Neurodegenerative diseases target large-scale human brain networks. Neuron 62, 42–52 (2009). This paper provides a description of how the patterns of neurodegeneration in different diseases reflect patterns of connectivity and large-scale neural systems.
Raj, A., Kuceyeski, A. & Weiner, M. A network diffusion model of disease progression in dementia. Neuron 73, 1204–1215 (2012).
Kfoury, N., Holmes, B. B., Jiang, H., Holtzman, D. M. & Diamond, M. I. Trans-cellular propagation of tau aggregation by fibrillar species. J. Biol. Chem. 287, 19440–19451 (2012).
Zhou, J., Gennatas, E. D., Kramer, J. H., Miller, B. L. & Seeley, W. W. Predicting regional neurodegeneration from the healthy brain functional connectome. Neuron 73, 1216–1227 (2012).
Jacobs, H. L. L. et al. Structural tract alterations predict down-stream tau accumulation in amyloid positive older individuals. Nat. Neurosci. 21, 424–431 (2018). This article provides compelling evidence for Aβ-facilitated spread of tau through the human episodic memory network.
Filippini, N. et al. Distinct patterns of brain activity in young carriers of the APOE-ε4 allele. Proc. Natl Acad. Sci. USA 106, 7209–7214 (2009).
Machulda, M. M. et al. Effect of APOE ε4 status on intrinsic network connectivity in cognitively normal elderly subjects. Arch. Neurol. 68, 1131–1136 (2011).
Grimmer, T. et al. Progression of cerebral amyloid load is associated with the apolipoprotein E ε4 genotype in Alzheimer’s disease. Biol. Psychiatry 68, 879–884 (2010).
Resnick, S. M. et al. Changes in Aβ biomarkers and associations with APOE genotype in 2 longitudinal cohorts. Neurobiol. Aging 36, 2333–2339 (2015).
Lim, Y. Y., Mormino, E. C. & Alzheimer’s Disease Neuroimaging Initiative. APOE genotype and early β-amyloid accumulation in older adults without dementia. Neurology 89, 1028–1034 (2017).
Mishra, S. et al. Longitudinal brain imaging in preclinical Alzheimer disease: impact of APOE ε4 genotype. Brain 141, 1828–1839 (2018).
Liu, C. C. et al. ApoE4 accelerates early seeding of amyloid pathology. Neuron 96, 1024–1032.e3 (2017).
Shi, Y. et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nature 549, 523–527 (2017).
Kantarci, K. et al. APOE modifies the association between Aβ load and cognition in cognitively normal older adults. Neurology 78, 232–240 (2012).
Wolk, D. A., & Dickerson, B. C. & Alzheimer’s Disease Neuroimaging Initiative. Apolipoprotein E (APOE) genotype has dissociable effects on memory and attentional-executive network function in Alzheimer’s disease. Proc. Natl Acad. Sci. USA 107, 10256–10261 (2010).
Chang, L. et al. Gray matter maturation and cognition in children with different APOE epsilon genotypes. Neurology 87, 585–594 (2016).
Schneider, J. A., Wilson, R. S., Bienias, J. L., Evans, D. A. & Bennett, D. A. Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology 62, 1148–1155 (2004).
de Groot, J. C. et al. Cerebral white matter lesions and cognitive function: the Rotterdam Scan Study. Ann. Neurol. 47, 145–151 (2000).
Price, T. R. et al. Silent brain infarction on magnetic resonance imaging and neurological abnormalities in community-dwelling older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Stroke 28, 1158–1164 (1997).
Gurol, M. E. et al. Cerebral amyloid angiopathy burden associated with leukoaraiosis: a positron emission tomography/magnetic resonance imaging study. Ann. Neurol. 73, 529–536 (2013).
Hedden, T. et al. Cognitive profile of amyloid burden and white matter hyperintensities in cognitively normal older adults. J. Neurosci. 32, 16233–16242 (2012).
Provenzano, F. A. et al. White matter hyperintensities and cerebral amyloidosis: necessary and sufficient for clinical expression of Alzheimer disease? JAMA Neurol. 70, 455–461 (2013).
Vemuri, P. et al. Vascular and amyloid pathologies are independent predictors of cognitive decline in normal elderly. Brain 138, 761–771 (2015).
Langbaum, J. B. et al. Blood pressure is associated with higher brain amyloid burden and lower glucose metabolism in healthy late middle-age persons. Neurobiol. Aging 33, 827.e11–827.e19 (2012).
Rodrigue, K. M. et al. Risk factors for β-amyloid deposition in healthy aging: vascular and genetic effects. JAMA Neurol. 70, 600–606 (2013).
Reed, B. et al. Associations between serum cholesterol levels and cerebral amyloidosis. JAMA Neurol. 71, 195–200 (2014).
Gottesman, R. F. et al. Association between midlife vascular risk factors and estimated brain amyloid deposition. JAMA 317, 1443–1450 (2017).
Vemuri, P. et al. Evaluation of amyloid protective factors and Alzheimer disease neurodegeneration protective factors in elderly individuals. JAMA Neurol. 74, 718–726 (2017).
Vemuri, P. et al. Age, vascular health, and Alzheimer disease biomarkers in an elderly sample. Ann. Neurol. 82, 706–718 (2017).
DeCarli, C. et al. Predictors of brain morphology for the men of the NHLBI twin study. Stroke 30, 529–536 (1999).
Mungas, D. et al. MRI predictors of cognition in subcortical ischemic vascular disease and Alzheimer’s disease. Neurology 57, 2229–2235 (2001).
Stern, Y. What is cognitive reserve? Theory and research application of the reserve concept. JINS 8, 448–460 (2002).
Head, D. et al. Exercise engagement as a moderator of the effects of APOE genotype on amyloid deposition. Arch. Neurol. 69, 636–643 (2012).
Brown, B. M. et al. Physical activity and amyloid-β plasma and brain levels: results from the Australian Imaging, Biomarkers and Lifestyle Study of Ageing. Mol. Psychiatry 18, 875–881 (2013).
Landau, S. M. et al. Association of lifetime cognitive engagement and low β-amyloid deposition. Arch. Neurol. 69, 623–629 (2012).
Wirth, M., Villeneuve, S., La Joie, R., Marks, S. M. & Jagust, W. J. Gene-environment interactions: lifetime cognitive activity, APOE genotype, and β-amyloid burden. J. Neurosci. 34, 8612–8617 (2014).
Vemuri, P. et al. Effect of intellectual enrichment on AD biomarker trajectories: longitudinal imaging study. Neurology 86, 1128–1135 (2016).
Spira, A. P. et al. Self-reported sleep and β-amyloid deposition in community-dwelling older adults. JAMA Neurol. 70, 1537–1543 (2013).
Sprecher, K. E. et al. Amyloid burden is associated with self-reported sleep in nondemented late middle-aged adults. Neurobiol. Aging 36, 2568–2576 (2015).
Mander, B. A. et al. β-amyloid disrupts human NREM slow waves and related hippocampus-dependent memory consolidation. Nat. Neurosci. 18, 1051–1057 (2015). This report describes relationships between slow-wave sleep, amyloid accumulation and memory loss that define a potential vicious cycle in an amyloid–sleep relationship.
Xie, L. et al. Sleep drives metabolite clearance from the adult brain. Science 342, 373–377 (2013).
Salter, M. W. & Stevens, B. Microglia emerge as central players in brain disease. Nat. Med. 23, 1018–1027 (2017).
Jonsson, T. et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N. Engl. J. Med. 368, 107–116 (2013).
Guerreiro, R. et al. TREM2 variants in Alzheimer’s disease. N. Engl. J. Med. 368, 117–127 (2013).
Kreisl, W. C. et al. In vivo radioligand binding to translocator protein correlates with severity of Alzheimer’s disease. Brain 136, 2228–2238 (2013).
Hamelin, L. et al. Early and protective microglial activation in Alzheimer’s disease: a prospective study using 18F-DPA-714 PET imaging. Brain 139, 1252–1264 (2016).
Parbo, P. et al. Brain inflammation accompanies amyloid in the majority of mild cognitive impairment cases due to Alzheimer’s disease. Brain 140, 2002–2011 (2017).
Villain, N. et al. Regional dynamics of amyloid-β deposition in healthy elderly, mild cognitive impairment and Alzheimer’s disease: a voxelwise PiB-PET longitudinal study. Brain 135, 2126–2139 (2012).
Jack, C. R. Jr. et al. Brain β-amyloid load approaches a plateau. Neurology 80, 890–896 (2013).
Duyckaerts, C. et al. PART is part of Alzheimer disease. Acta Neuropathol. 129, 749–756 (2015).
La Joie, R. et al. Region-specific hierarchy between atrophy, hypometabolism, and β-amyloid (Aβ) load in Alzheimer’s disease dementia. J. Neurosci. 32, 16265–16273 (2012).
Giasson, B. I. et al. Initiation and synergistic fibrillization of tau and α-synuclein. Science 300, 636–640 (2003).
Botha, H. et al. FDG-PET in tau-negative amnestic dementia resembles that of autopsy-proven hippocampal sclerosis. Brain 141, 1201–1217 (2018).
Clark, C. M. et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol. 11, 669–678 (2012).
Sabri, O. et al. Florbetaben PET imaging to detect amyloid β plaques in Alzheimer’s disease: phase 3 study. Alzheimers Dement. 11, 964–974 (2015).
Curtis, C. et al. Phase 3 trial of flutemetamol labeled with radioactive fluorine 18 imaging and neuritic plaque density. JAMA Neurol. 72, 287–294 (2015).
Schonhaut, D. R. et al. 18F-flortaucipir tau positron emission tomography distinguishes established progressive supranuclear palsy from controls and Parkinson disease: a multicenter study. Ann. Neurol. 82, 622–634 (2017).
Wirth, M. et al. Alzheimer’s disease neurodegenerative biomarkers are associated with decreased cognitive function but not β-amyloid in cognitively normal older individuals. J. Neurosci. 33, 5553–5563 (2013).
Maass, A. et al. Comparison of multiple tau-PET measures as biomarkers in aging and Alzheimer’s disease. Neuroimage 157, 448–463 (2017).
Acknowledgements
Research described in this article was supported in part by US National Institutes of Health grants AG034570, AG045611 and AG019724. The author is indebted to R. La Joie, S. Landau, A. Maass and G. Rabinovici for their thoughtful comments.
Reviewer information
Nature Reviews Neuroscience thanks K. Josephs, P. Matthews and M. Rossor for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author serves as a consultant to BioClinica, Novartis and Genentech.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Aβ plaques
-
Also termed neuritic or senile plaques, Aβ plaques are one of the pathological hallmarks of AD and are composed of aggregates of the Aβ protein that are found at postmortem examination of the brain.
- Neurofibrillary tangles
-
The other major pathological hallmark of AD, they are composed of aggregated forms of hyperphosphorylated tau protein as intraneuronal paired helical filaments.
- Mild cognitive impairment
-
(MCI). An intermediate stage between normal cognition and dementia; individuals with MCI usually experience amnesia and are at increased risk of developing AD.
- Amyloid cascade hypothesis
-
A dominant hypothesis in the AD research field proposing that Aβ generation is the inciting event that leads to subsequent downstream processes of tau deposition and neurodegeneration, eventuating in dementia.
- Default-mode network
-
(DMN). A canonical resting-state network of the brain that is active when individuals are not engaged in attending to or responding to external stimuli.
- Hubs
-
Brain regions (or nodes) that have many connections to other brain regions and serve as areas of convergence of information from multiple processing streams.
- Rich club
-
A group of brain regions (or nodes) that are highly connected to one another and that show a high degree of hub-like connectivity to many other brain regions.
- Braak neuropathological staging
-
A widely adopted method of classification of tau pathology based on cross-sectional autopsy data that proposes a progression of tau neurofibrillary pathology from the MTL (Braak stages I/II) through a limbic stage (III/IV) to a diffuse neocortical stage (V/VI).
- Apolipoprotein E
-
(APOE). A polymorphic gene with three alleles; the APOE ε4 allele is a risk factor for LOAD.
- Suspected non-Alzheimer pathophysiology
-
(SNAP). A descriptive term for evidence of neurodegeneration in the absence of biomarker evidence of Aβ.
- Primary age-related tauopathy
-
(PART). An autopsy finding reflecting neurofibrillary tau pathology in the absence of Aβ pathology; fairly common in older people and with an unknown relationship to AD.
- Cognitive reserve
-
A hypothetical construct proposing differences in individual susceptibility to account for why people with similar levels of disease pathology show different levels of cognitive ability.
Rights and permissions
About this article
Cite this article
Jagust, W. Imaging the evolution and pathophysiology of Alzheimer disease. Nat Rev Neurosci 19, 687–700 (2018). https://doi.org/10.1038/s41583-018-0067-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41583-018-0067-3
This article is cited by
-
Impaired long-range excitatory time scale predicts abnormal neural oscillations and cognitive deficits in Alzheimer’s disease
Alzheimer's Research & Therapy (2024)
-
Associations between cardiometabolic multimorbidity and cerebrospinal fluid biomarkers of Alzheimer’s disease pathology in cognitively intact adults: the CABLE study
Alzheimer's Research & Therapy (2024)
-
Diverse Efficacy of Dimethyl Fumarate in Alleviating the Late Streptozotocin-Induced Cognitive Impairment and Neuropathological Features in Rat
Molecular Neurobiology (2024)
-
Impact of APOE on amyloid and tau accumulation in argyrophilic grain disease and Alzheimer’s disease
Acta Neuropathologica Communications (2024)
-
Biomarker-based staging of Alzheimer disease: rationale and clinical applications
Nature Reviews Neurology (2024)