Abstract
The search for reconsolidation blockers may uncover clinically relevant drugs for disrupting memories of significant stressful life experiences, such as those underlying the posttraumatic stress disorder. Considering the safety of systemically administered cannabidiol (CBD), the major non-psychotomimetic component of Cannabis sativa, to animals and humans, the present study sought to investigate whether and how this phytocannabinoid (3–30 mg/kg intraperitoneally; i.p.) could mitigate an established memory, by blockade of its reconsolidation, evaluated in a contextual fear-conditioning paradigm in rats. We report that CBD is able to disrupt 1- and 7-days-old memories when administered immediately, but not 6 h, after their retrieval for 3 min, with the dose of 10 mg/kg being the most effective. This effect persists in either case for at least 1 week, but is prevented when memory reactivation was omitted, or when the cannabinoid type-1 receptors were antagonized selectively with AM251 (1.0 mg/kg). Pretreatment with the serotonin type-1A receptor antagonist WAY100635, however, failed to block CBD effects. These results highlight that recent and older fear memories are equally vulnerable to disruption induced by CBD through reconsolidation blockade, with a consequent long-lasting relief in contextual fear-induced freezing. Importantly, this CBD effect is dependent on memory reactivation, restricted to time window of <6 h, and is possibly dependent on cannabinoid type-1 receptor-mediated signaling mechanisms. We also observed that the fear memories disrupted by CBD treatment do not show reinstatement or spontaneous recovery over 22 days. These findings support the view that reconsolidation blockade, rather than facilitated extinction, accounts for the aforementioned CBD results in our experimental conditions.
Similar content being viewed by others
INTRODUCTION
In contrast to the traditional view that memory formation is a one-time process of consolidation, converging evidence suggests that memories are dynamically stored and reprocessed each time they are reactivated (Misanin et al, 1968; Nader et al, 2000; Eisenberg et al, 2003; Dudai, 2006; Alberini, 2011). The retrieval of a fear memory induced by reexposure to the conditioned context without the unconditioned stimulus presentation may trigger reconsolidation or extinction (Suzuki et al, 2004; Lee et al, 2006). An important aspect influencing the outcome of memory reactivation is the duration of the retrieval session, whereas a brief (1.5–5 min) reexposure to the conditioned context favors reconsolidation and preserves the fear response, a prolonged session (of 10 min or more) tends to cause extinction, resulting in attenuation of fear responses (Bustos et al, 2006, 2009).
Several drugs have been shown to impair both reconsolidation and extinction of a contextual fear memory in laboratory animals upon systemic administration. Examples are the β-adrenergic antagonist propranolol (Debiec and Ledoux, 2004; Mueller et al, 2008) and midazolam, a benzodiazepine that positively modulates the γ-amino butyric acid type-A receptor function (Bustos et al, 2006, 2009). Similarly, disruption in memory reconsolidation and extinction have been reported following the infusion of protein synthesis inhibitors into the dorsal hippocampus (Lee et al, 2004; Rodriguez-Ortiz et al, 2008) or the ventromedial prefrontal cortex (Akirav and Maroun, 2006; Akirav et al, 2006), as well as after microinjections of inhibitors of the mitogen-activated protein kinase pathway into the amygdala (Duvarci et al, 2005; Herry et al, 2006). From a clinical perspective, however, it would seem important to identify drugs that could disrupt the reconsolidation of fear memories, but facilitate their extinction (Yamada et al, 2009), as both these processes are thought to be implicated in pathological conditions such as the posttraumatic stress disorder (Yehuda et al, 2010).
Cannabidiol (CBD), a phytocannabinoid with a remarkably safe profile for use in humans (Nurmikko et al, 2007), has been shown to facilitate extinction of a contextual fear memory in rats by a mechanism that involves activation of cannabinoid type-1 receptors (Bitencourt et al, 2008). This finding agrees with extensive evidence indicating that the endocannabinoid system, acting through the same type of receptors, modulates memory reconsolidation of fearful events (Lin et al, 2006; Kobilo et al, 2007; de Oliveira Alvares et al, 2008; Suzuki et al, 2008). It is unknown, however, whether CBD could also interfere with the reconsolidation of aversive memories.
The objective of the present study was to assess the potential disruptive effect of the CBD, as well as to determine its underlying mechanism, on fear memory in rats. We demonstrate that CBD is able to disrupt recent and older contextual fear memories by interfering with their reconsolidation, and that such effect is long lasting and can be prevented by pharmacological antagonism of cannabinoid type-1 receptors.
MATERIALS AND METHODS
Animals
Experiments were performed in male Wistar rats (bred and raised by the animal house of the Federal University of Santa Catarina, Florianopolis, Brazil) weighing 300–350 g and aged 14–16 weeks. The animals were housed in groups of four per cage (50 × 30 × 15 cm), kept on a 12-h light/dark cycle (lights on at 0700 hours) and received food and water ad libitum. All procedures were approved by the Institutional Ethical Committee for the care and use of laboratory animals of the Federal University of Santa Catarina (23080.016341/2010-30) in compliance with guidelines of the Brazilian Society of Neuroscience and Behavior and Brazilian legislation.
Drugs
Cannabidiol (THC-Pharma, Germany; 3–30 mg/kg) and AM251 (Tocris, USA; 1.0 mg/kg) were dissolved in NaCl 0.9% containing 5% of polyoxyethylene sorbitan monooleate (Vetec, Brazil). WAY100635 (Sigma, USA; 0.1 mg/kg) was dissolved in NaCl 0.9%. The choice of doses was based on previously published studies where AM251 and WAY100635 prevented the behavioral effects of the CBD after systemic injection (Resstel et al, 2009; Casarotto et al, 2010). Moreover, as antagonism of cannabinoid type-1 receptors has been shown to enhance fear memory reconsolidation (de Oliveira Alvares et al, 2008) and to decrease anysomycin-induced amnesic effects (Suzuki et al, 2008) per se, we opted for using a low dose of AM251 in order to minimize the potential impact of this potentially confounding effect. Midazolam (Cristalia, Brazil) was diluted in NaCl 0.9% and administered at a putative memory-impairing dose (1.5 mg/kg; Bustos et al, 2006, 2009) in the first two experiments to serve as a positive control. All solutions were prepared immediately before use and injected i.p. in a volume of 1.0 ml/kg.
Apparatus
Fear conditioning was assessed in a rectangular chamber (35 × 20 × 30 cm), with aluminum sidewalls and a front wall and ceiling-door made of Plexiglas, which will be designated herein as Context A. Its grid floor, made of stainless steel bars (3 mm diameter, spaced 9 mm apart center-to-center), was connected to a circuit board and a shock generator (Insight, Ribeirão Preto, Brazil) to enable delivery of controlled electrical footshocks as detailed in the procedure section. A second rectangular chamber (33 × 25 × 33 cm), designated herein as Context B, was made of glass and had a grid lid and transparent walls and floor, to provide contextual cues as different as possible from those of Context A used for conditioning. Importantly, Context B was used as a neutral context unable to induce fear memory reactivation. A third chamber (40 × 25 × 30 cm), which clearly differed from Context A in terms of internal (color of sidewalls) and external (room) cues and designated herein as Context C, was used in experiment 4.
General Procedures and Data Collection
Behavioral testing was always carried out under low-intensity illumination (70 lux) from 1300 to 1700 hours, ie, during the diurnal phase. In all experiments, each animal was placed in Context A and allowed to freely explore it for 3 min, as an initial familiarization session, and returned to its home cage. On the next day, the animal was again placed in Context A for the conditioning session during which it received, after an initial 30 s delay (pre-shock period), the unconditioned stimulus (three electrical footshocks of 0.7 mA, 60 Hz, for 3 s, with a 30 s intertrial period). The animal remained in this chamber for an additional 30 s (post-shock period) before its return to its home cage. In the reactivation session (conducted at different intervals after the conditioning session, depending on the experiment), the animal was reexposed to Context A (the conditioning chamber) for 3 min without presentation of the unconditioned stimulus, so as to induce the retrieval/reactivation of the established fear memory. In Test A, the animal was reexposed to Context A for 3 min in the absence of unconditioned stimulus presentation, whereas in Test B it was exposed to Context B (ie, the neutral chamber; unpaired context) also for 3 min. After each behavioral session, both chamber types were cleaned with a tissue paper soaked with 10% ethanol-water solution. The experimenter was unaware of the treatment condition in all studies.
Freezing behavior, a commonly used index of fear in rats (Blanchard and Blanchard, 1969) and defined as a total absence of body and head movements, except those associated with breathing, was continuously recorded during the experimental sessions by a video camera. The freezing time in each period was quantified (in seconds) using a stopwatch and expressed as the percentage of total session time.
Statistical Analysis
Results are expressed as mean±SEM. After ensuring the assumptions of normality and homoscedasticity, the percentage of freezing time observed in Context A (reactivation session, Test A, Test A1, Test A2, and/or reinstatement) and Context B (no reactivation session, Test B, Test B1, and/or Test B2) were submitted to separated one-way or repeated-measures analysis of variance (ANOVA). The Newman–Keuls test was used for post-hoc comparisons. The statistical significance level was set at P<0.05.
RESULTS
Experiment 1: CBD Disrupts Fear Memory Through Reconsolidation Blockade
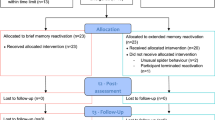
To investigate whether CBD would affect the reconsolidation of a 1-day-old fear memory, 51 contextually conditioned rats were randomly allocated to five groups (n=7–12 per group) based on the systemic treatment (vehicle, 3, 10, or 30 mg/kg of CBD, or 1.5 mg/kg of midazolam) given immediately after memory retrieval.
Repeated-measures ANOVA showed a significant drug treatment × Context A reexposure interaction (F(4,46)=3.9; P<0.01). As shown in Figure 1a, all groups presented a similar high freezing time in the reactivation session. However, during reexposure to the paired context (Test A), both CBD- and midazolam-treated animals expressed significantly less freezing than controls, suggesting that these drug treatments induced a failure in memory reconsolidation. Moreover, one-way ANOVA did not show significant drug treatment effects during Test B performed 24 h after the reactivation session (F(4,46)=0.95; P=0.40). All groups expressed a similar low freezing time when exposed to the neutral Context B (Figure 1a).
(a) Evidence for a disruptive effect of cannabidiol (CBD) or midazolam (MDZ) on fear memory through reconsolidation blockade. After a familiarization period, animals were conditioned to Context A by receiving three footshocks, the unconditioned stimulus (US). On the next day, they were reexposed to Context A for 3 min to reactivate the established fear memory. Immediately after this period, they received intraperitoneal injections of vehicle (VEH), CBD (3–30 mg/kg), or MDZ (1.5 mg/kg). Both CBD- and MDZ-treated animals froze less than controls when reexposed to the conditioned context (Test A) 24 h later. No difference was found when the animals were exposed to a neutral context (Test B). (b) Memory reactivation is necessary for the disruptive effect of CBD or MDZ on fear memory to occur. On the day following the contextual conditioning session described above, the animals were treated with vehicle (VEH), CBD (10 mg/kg), or MDZ (1.5 mg/kg) after being exposed to the neutral context B for 3 min (unpaired context). No differences were found when they were reexposed to the paired context 24 h later (Test A). The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. The asterisks indicate a significant difference (P<0.05) from respective controls, whereas the hash (fence) symbol indicates significant difference from other groups treated with CBD.
To further examine the disruptive effect of these drugs on fear memory, the most effective dose of CBD (10 mg/kg) or midazolam (1.5 mg/kg) was administered to independent groups of contextually conditioned rats (n=6–7 per group) after their exposure to Context B, a neutral context different from that used for conditioning (no reactivation session). One-way ANOVA showed no significant drug effect in this session (F(2, 17)=2.4; P=0.12) and in Test A (F(2, 17)=0.57; P=0.58) performed 24 h later. CBD- and midazolam-treated groups froze for just as much time as controls in both cases (Figure 1b), suggesting that the reconsolidation blockade induced by these drugs depends on prior memory reactivation.
Experiment 2: Delayed CBD Treatment Spares Fear Memory from Disruption
Memory reconsolidation is a gradual process that takes up to 6 h after retrieval to be completed (Schafe and LeDoux, 2000; Dudai, 2004). To examine whether CBD-induced disruption of fear memory is specific to the reconsolidation phase, 21 contextually conditioned rats (n=7 per group) were randomly allocated to receive CBD, midazolam, or vehicle at 6 h after memory retrieval.
Repeated-measures ANOVA revealed neither a drug treatment × Context A reexposure interaction (F(2, 18)=0.72; P+0.50) nor significant main effects of these factors (F(2, 18)=0.32; P=0.73 and F(1, 18)=1.61; P=0.22, respectively). As shown in Figure 2, both CBD- and midazolam-treated animals behaved like controls, exhibiting high freezing times during reactivation and Test A, suggesting that disruption of fear memory induced by these drugs is no longer seen when they are administered after completion of the reconsolidation process. As with experiment 1, these groups had a similar low freezing time on Test B (F(2, 18)=0.63; P=0.54).
Fear memory disruption induced by cannabidiol (CBD) or midazolam (MDZ) is restricted to the time window in which reconsolidation takes place. On the day following the contextual conditioning session described in Figure 1, the animals were reexposed to Context A for 3 min to reactivate the fear memory. Six hours later, they received intraperitoneal injections of vehicle (VEH), CBD (10 mg/kg), or MDZ (1.5 mg/kg). Neither CBD- nor MDZ-treated animals froze less than controls during Test A performed 24 h later. The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. No statistically significant differences between groups were detected in this experiment.
Experiment 3: CBD-induced Fear Memory Disruption Does not Show Spontaneous Recovery Over 22 Days
Reexposure to the conditioned context without reinforcement may lead to extinction. Although it has been shown that a 3-min memory retrieval session favors the reconsolidation process (Bustos et al, 2009), it is possible that, under our experimental conditions, the reduction in freezing time induced by CBD demonstrated in experiment 1 involves facilitated extinction. As spontaneous recovery may occur over the course of a few weeks after fear memory extinction (Lattal and Abel, 2004), we attempted to rule out this possibility by investigating whether fear memory would reappear with the passage of time. To this aim, 25 contextually conditioned rats were treated with CBD (10 mg/kg) or vehicle immediately after memory retrieval, and reexposed to Context A at either 1 and 8 or 1 and 22 days later (n=6–7 per group).
Repeated-measures ANOVA showed significant drug treatment effects in these selected intervals of time between the first and second Test A (7 days: F(1, 11)=25.9; P<0.001; 21 days: F(1, 10)=11.4; P<0.01). As shown in Figure 3, CBD-treated animals expressed significantly less freezing than controls in both reexposures to Context A. More importantly, whereas the CBD group presented a low freezing time on the second Test A, comparable to that seen on the first test (P=0.58 and 0.72, respectively), vehicle-treated animals showed a similar high freezing time on the second Test A when compared both with the first Test A (P=0.93 and 0.32, respectively) or to the reactivation session (P=0.10 and 0.23, respectively). Taken together, these results corroborate that a 3-min memory retrieval session favored reconsolidation, and suggest the spontaneous recovery from the CBD-induced fear memory disruption does not occur at least over the first 22 days.
Fear memory that failed to reconsolidate after cannabidiol (CBD) administration does not recover spontaneously over 22 days. On the day following the contextual conditioning session in Context A (described in Figure 1), the animals were reexposed to this chamber for 3 min to reactivate the established fear memory and then administered with vehicle (VEH) or CBD (10 mg/kg). A second Test A was performed 7 (a) or 21 (b) days after the first one. Whereas the CBD-treated group maintained a reduced freezing response on both reexposures to the conditioned context, vehicle-treated animals presented a high freezing time in these sessions similar to that seen during reactivation. The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. The asterisk indicates significant difference (P<0.05) from respective controls, and NS denotes a not statistically significant difference.
Experiment 4: CBD-induced Fear Memory Disruption Does not Show Reinstatement
Another approach used to show that fear memory survives extinction is to present the unconditioned stimulus in the absence of the conditioned stimulus, as a reminder to reinstate the extinguished conditioned response. To confirm preceding results suggesting that CBD interfered with memory reconsolidation rather than extinction in our experimental conditions, we evaluated whether exposure to a mild footshock in a distinct context would reinstate freezing when fear to the Context A was tested again. To this aim, 19 contextually conditioned rats were randomly allocated to two groups (n=9–10 per group) based on the systemic treatment (vehicle or 10 mg/kg of CBD) administered immediately after memory retrieval. Both groups underwent extinction for 10 min in Context A 48 h later. On the next day, animals were exposed to Context C for 30 s (pre-shock period), then received a single footshock of 0.3 mA, 60 Hz, for 3 s, and continued in this chamber for more 30 s (post-shock period). Twenty-four hours after this footshock reminder session in Context C, animals were subjected to a test of memory reinstatement that consisted of a 5-min exposure to the Context A.
Repeated-measures ANOVA showed a significant drug treatment × context A reexposure interaction (F(3, 51)=3.6; P<0.05). As shown in Figure 4, all groups presented a similar high freezing time in the reactivation session, but CBD-treated animals expressed a significantly less freezing during Test A than controls. This difference was abolished (P=0.28) with the fear extinction session. When reexposed to Context A 1 day after a footshock reminder session in Context C, vehicle- but not CBD-treated animals reinstated the extinguished conditioned response. This result confirms that CBD affected the reconsolidation process. Moreover, one-way ANOVA did not show significant drug treatment effects during Test B performed 24 h later (F(1, 17)=0.01; P=0.97). Both groups expressed a low freezing time when exposed to the Context B (Figure 4).
Fear memory that failed to reconsolidate after cannabidiol (CBD) administration does not show reinstatement. On the day following the contextual conditioning session in Context A (described in Figure 1), the animals were reexposed to Context A for 3 min to reactivate the established fear memory and then treated with vehicle (VEH) or CBD (10 mg/kg). In comparison with controls, CBD-treated animals froze less in Test A performed 24 h later. Both groups were submitted, 24 h later, to the extinction of fear memory in Context A for 10 min. Accordingly, their level of freezing behavior was no longer different in this session. On the next day, animals were exposed to Context C for 1 min where they received a single lower-intensity reminder footshock (US). Twenty-four hours later, they were tested for memory reinstatement, being reexposed to the conditioned context for 5 min. During this session, controls showed a higher freezing time than CBD-treated animals. Both groups, however, behaved similarly in a neutral context (Test B). The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. The asterisk indicates significant difference (P<0.05) from respective controls, the hash (fence) symbol indicates significant difference from the same group during Test A, the plus symbol indicates significant difference from the same group during extinction, and NS denotes a not statistically significant difference.
Experiment 5: Fear Memory Disruption Induced by CBD is Long Lasting
To examine whether CBD could induce a persistent disruption of fear memory through reconsolidation blockade, 19 contextually conditioned rats (n=8–11 per group) were treated immediately after memory retrieval with 10 mg/kg of this drug or vehicle and reexposed to Context A 1 week later.
Repeated-measures ANOVA showed a significant drug treatment × Context A reexposure interaction (F(1, 17)=24.5; P<0.001). As shown in Figure 5a, these groups presented a similar high freezing time in the reactivation session, but CBD-treated animals expressed a significantly less freezing during reexposure to the paired context (Test A) than controls, suggesting that the disruptive effect of this drug on fear memory is long lasting. One-way ANOVA did not show any significant drug effect during Test B performed 24 h later (F(1, 17)=0.27; P=0.61). These groups had a similar low freezing time when exposed to the neutral Context B (Figure 5a).
(a) Disruption of fear memory induced by cannabidiol (CBD) treatment is long lasting and context-specific. On the day following the contextual conditioning session in Context A (described in Figure 1), the animals were reexposed to Context A for 3 min to reactivate the established fear memory and then treated with vehicle (VEH) or CBD (10 mg/kg). CBD-treated animals froze less than controls when reexposed to the conditioned context (Test A) 1 week later. However, when memory reactivation was omitted (b), this result was no longer observed. The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. The asterisk indicates significant difference (P<0.05) from respective controls.
In addition, as shown in an additional experiment with independent groups (n=7 per group) of contextually conditioned rats (Figure 5b), administration of CBD at 10 mg/kg immediately after exposure to Context B failed to change freezing relative to controls when the animals were reexposed to the conditioned context (Test A) 7 days later (F(1, 12)=0.70; P=0.43). This reinforces the view that memory reactivation is a pivotal requirement for the occurrence of CBD's long lasting disruptive effect on fear memory.
Experiment 6: An Older Fear Memory is Equally Disrupted by CBD Treatment
To investigate whether CBD would also affect the reconsolidation of older fear memories, 17 contextually conditioned rats were randomly allocated to two groups (n=8–9 per group) treated with vehicle or 10 mg/kg of CBD, immediately after retrieving a fear memory acquired 7 days earlier.
Repeated-measures ANOVA showed a significant drug treatment × Context A reexposure interaction (F(2, 28)=10.5; P<0.001). As shown in Figure 6, vehicle- and CBD-treated groups displayed a high and comparable (P=0.40) freezing time in the reactivation session, but the latter group froze significantly less than controls in both the first and the second sessions of reexposure to the paired Context A (Test A) performed 1 week later. These results indicate that a 7-day-old fear memory is also susceptible to disruption by CBD, and that this effect persists for at least 8 days. Moreover, repeated-measures ANOVA revealed neither a significant drug treatment × Context B reexposure interaction (F(1, 15)=0.22; P=0.66) nor significant main effects of these factors (F(1, 15)=4.3; P=0.06 and F(1, 15)=0.14; P=0.71, respectively). These groups expressed a similar low freezing time when exposed to Context B at either 2 (P=0.36) or 9 (P=0.32) days after memory reactivation and drug treatment (Figure 6).
A 7-day-old fear memory is also susceptible to disruption by cannabidiol (CBD). One week after the contextual conditioning session in Context A (described in Figure 1), the animals were reexposed to this chamber for 3 min to reactivate the fear memory, and immediately after received vehicle (VEH) or CBD (10 mg/kg). CBD impaired reconsolidation of the fear memory, which was evident during the reexposure to Context A (Test A) 24 h later. A similar effect of CBD effect was also present in a second Test A conducted 1 week later. No difference was found when animals were exposed to Context B (unpaired context). The arrowhead indicates the moment of drug treatment. Bars represent the percentage of freezing time. The asterisk indicates significant difference (P<0.05) from respective controls, and NS denotes a not statistically significant difference.
Experiment 7: CBD-induced Disruption of Fear Memory Depends on Activation of Cannabinoid Type-1 Receptors
To elucidate how CBD disrupts fear memory, 52 contextually conditioned rats were randomly allocated to six groups (n=8–9 per group) and treated systemically with vehicle, 0.1 mg/kg of the serotonin type-1A receptor antagonist WAY100635, or 1.0 mg/kg of the cannabinoid type-1 receptor antagonist AM251, immediately after memory retrieval. Thirty minutes later, they were given a second systemic injection of either vehicle or 10 mg/kg of CBD. In vivo studies with radiolabeled WAY100635 and AM251 indicate that this 30-min period is adequate to ensure significant brain levels of either drug (Gatley et al, 1996; Pike et al, 1998), ie, at the time animals received the second treatment.
Repeated-measures ANOVA showed a significant drug pretreatment × drug treatment interaction (F(2, 46)=3.3; P<0.05). As shown in Figure 7, all groups presented a similar high freezing time in the reactivation session. During Test A, vehicle-pretreated animals administered with CBD froze significantly less than the respective controls. This difference was also observed when the WAY100635-CBD group was compared with the WAY100635-vehicle group. In AM251-pretreated animals, however, the reduction in freezing time induced by CBD administration after memory reactivation was no longer observed. This suggests that cannabinoid type-1 receptors, rather than serotonin type-1A receptors, mediate the disruptive effect of CBD on fear memory. All groups expressed an equivalent low freezing time when exposed to the neutral Context B (F(2, 46)=0.31; P=0.74) (Figure 7).
Disruption of fear memory by cannabidiol (CBD) is mediated by cannabinoid type-1 rather than serotonin type-1A receptors. One day after the contextual conditioning session in Context A (described in Figure 1), the animals were reexposed to this chamber for 3 min to reactivate the fear memory, and immediately after pretreated with vehicle (VEH), 0.1 mg/kg of the serotonin type-1A receptor antagonist WAY100635 (WAY) or 1.0 mg/kg of the cannabinoid type-1 receptor antagonist AM251 (AM). Thirty min later, they received VEH or CBD (10 mg/kg). Both VEH-CBD and WAY-CBD groups froze less than respective controls when reexposed to the conditioned context (Test A) 24 h later. The AM251-CBD group, however, was not different from the respective control, showing a high level of freezing. No differences were found when the animals were exposed to a neutral context (Test B). Arrowheads indicate the moment of drug pretreatment and treatment. The asterisk indicates significant difference (P<0.05) from respective controls.
DISCUSSION
Fear-conditioned rats reexposed to the paired context spent substantial amount of time in freezing behavior. This result agrees with a wealth of evidence showing reliable emotional responses in the contextual fear-conditioning paradigm (Fanselow, 2010; Lee, 2010). In contrast, these animals exhibited a low freezing time when exposed to a neutral context, confirming that only cues associated with the specific conditioned context are able to induce memory retrieval (Sara, 2000; Bustos et al, 2006). Moreover, using 3-min-long retrieval sessions, the current study found that reexposure to the conditioned context for more than once failed to induce fear memory extinction, a result consistent with a previous demonstration that sessions lasting for at least 10 min are required in order to elicit this process successfully (Bustos et al, 2009).
The U-shaped dose–response curve to the inhibitory effect of CBD, administered immediately after memory reactivation, on the freezing response exhibited by rats upon subsequent reexposure to the conditioned context indicated that, at 10 mg/kg, the drug exerted its greatest disruptive effect on fear memory through blockade of reconsolidation. Likewise, we observed that midazolam also impaired this process when given soon after the reactivation session, a result that confirms a previous report (Bustos et al, 2006) and adds further support for the effectiveness of the current protocol to investigate reconsolidation of contextual fear memories. If the disruptive effect of these drugs on fear memory depends on briefly retrieving its trace, one would expect that without exposure to the retrieval session the conditioned fear response would be unchanged. Indeed, when given after a 3-min exposure to a neutral context, neither CBD nor midazolam interfered with freezing time on the subsequent reexposure to the conditioning chamber.
As systemic administration of CBD has been shown to attenuate unconditioned and conditioned fear-related responses in rodents (Guimarães et al, 1990; Moreira et al, 2006; Resstel et al, 2009; Casarotto et al, 2010), the reduction in freezing time seen during Test A performed 24 h after its administration could also have resulted from a long-lasting anti-aversive effect of this phytocannabinoid. Nevertheless, as the concentration of CBD in the brain reaches its maximal level at 2 h after i.p. administration to rats and is completely eliminated over the first 24 h (Deiana et al, 2012), this possibility is unlikely. Substantiating this assumption, CBD failed to change freezing time in the non-reactivated group.
Convergent evidence indicates that the susceptibility of memory to pharmacological manipulations after retrieval is restricted to a limited time window. Drug effects on reconsolidation are usually observed when they are given between 0 and 3 h after reactivation session (Przybyslawski et al, 1999; Bustos et al, 2006; Boccia et al, 2011). Accordingly, in the present study the disruptive effects of CBD and midazolam on fear memory were observed when each drug was administered immediately after retrieval, but not 6 h later. This result reinforces the view that drug interference on the reconsolidation process is specific, as no disruptive effect on fear memory was observed at a time point when this process had already been completed. Moreover, the absence of changes in freezing time of animals reexposed to the conditioning context 18 h after being treated with CBD or midazolam also rules out the possibility that their anti-aversive action could explain the results observed in experiment 1.
Bitencourt et al (2008) have shown that CBD can facilitate the extinction of contextual fear memory in rats. Despite the differences in procedures adopted in our study and theirs, namely the duration of reactivation sessions (3 vs 9 min), drug regimen (single vs repeated injections), and route of drug administration (i.p. vs i.c.v.), the reduction induced by CBD in freezing behavior seen during reexposure to conditioning context could have resulted from interference with the extinction process. Of relevance to the present discussion is the fact that after extinction of the original fear memory, it may progressively reemerge, a phenomenon known as spontaneous recovery (Rescorla, 2004). In the present study, no behavioral evidence for the recovery of fear memory was seen at 8 or 22 days after CBD had been given to interfere in post-memory reactivation. These results are in agreement with previous studies showing the absence of spontaneous recovery within the period of 7–24 days, following disruption of memory reconsolidation, in tasks such as inhibitory avoidance, contextual, and auditory fear conditioning (Duvarci and Nader, 2004; Bustos et al, 2006; Taubenfeld et al, 2009). They also reinforce the suggestion that CBD interfered with the reconsolidation of fear memory rather than its extinction in our experimental conditions. Such evidence is supported by the experiment in which the application of a reminder footshock did not result in the reinstatement of the fear memory that had been disrupted earlier by the CBD-induced blockade of reconsolidation.
Multiple mechanisms have been related to the behavioral effects of CBD (Izzo et al, 2009), including facilitation of cannabinoid type-1 and serotonin type-1A receptor-mediated signaling (Bitencourt et al, 2008; Moreira et al, 2006; Campos and Guimarães, 2008; Resstel et al, 2009). The former possibly involves the inhibition of uptake and degradation of anandamide, leading to an indirect facilitation of endocannabinoid neurotransmission (Bisogno et al, 2001; Izzo et al, 2009), whereas the latter could depend on direct activation of serotonin type-1A receptors (Russo et al, 2005). In our study, pretreatment with AM251, a selective cannabinoid type-1 receptor antagonist, but not with the serotonin type-1A receptor antagonist WAY100635, was able to prevent the disruption of fear memory by CBD. This finding, which implicates the cannabinoid type-1 receptor in the effects of CBD, is consistent with results demonstrating that reconsolidation of fear memory in rodents is blocked by the activation of these receptors in the hippocampus, amygdala, and cortex (Lin et al, 2006; Kobilo et al, 2007; de Oliveira Alvares et al, 2008; Suzuki et al, 2008). As cannabinoid type-1 receptors are highly expressed in these interconnected brain areas implicated in aversive memory reconsolidation (Herkenham et al, 1990; Debiec et al, 2002, 2006; Lee et al, 2004; Akirav and Maroun, 2006), these brain sites could potentially be the ones responsible for the effects of CBD on this process. Even if serotonin type-1A receptors have also been involved in aversive memory reconsolidation (Ogren et al, 2008), the failure of the WAY100635 to prevent the effects of CBD suggests that cannabinoid type-1 rather than serotonin type-1A receptors mediate the disruptive effect of CBD on fear memory. However, as the current study only tested the effects of single doses of these antagonists, future experiments to discard other possible explanations such as pharmacokinetic interaction or ineffective drug concentration would seem advisable. In addition to its interference with cannabinoid type-1 and serotonin type-1A receptor-mediated signaling mechanisms, other effects of CBD have been ascribed to different mechanisms (Izzo et al, 2009). Among them, it was demonstrated that CBD, along with anandamide, can also activate transient receptor potential vanilloid type-1 channels (Bisogno et al, 2001). However, the involvement of these other mechanisms of action in memory reconsolidation is still unknown.
Blockade of reconsolidation by CBD of a fear memory retrieved 7 days after conditioning was also shown in the current study. This result agrees with a report that reconsolidation of a 2-day-old contextual fear memory was impaired after activation of cannabinoid type-1 receptors in the rat hippocampus (De Oliveira Alvares et al, 2008), and substantiates the role of the endocannabinoid system in the process of memory reconsolidation (Lin et al, 2006; Kobilo et al, 2007; Suzuki et al, 2008). When the time between conditioning and retrieval is longer than 1 week, memories tend to become less vulnerable to intervention (Milekic and Alberini, 2002). Accordingly, midazolam blocks reconsolidation of contextual fear memory in rats when it is administered after a retrieval session conducted 7 days after the conditioning session, but not if it is conducted at 21 or 36 days (Bustos et al, 2009). In this regard, it is possible that older memories undergo reconsolidation with longer retrieval sessions (Suzuki et al, 2004; Bustos et al, 2010). It is unknown, however, whether CBD-induced blockade of reconsolidation would still be evident to a fear memory retrieved under these conditions.
Considering the present results with CBD, allied to its facilitatory effect on extinction of fear memory (Bitencourt et al, 2008), the lack of negative psychotropic effects such as sedation when it is systemically administered to humans even in high doses (Bhattacharyya et al, 2009), and its clinical anxiolytic potential in humans (Bergamaschi et al, 2011), this phytocannabinoid could constitute a potentially useful drug to target the cognitive and emotional processes associated with posttraumatic stress disorder. Indeed, treating patients suffering from this anxiety disorder with drugs that manipulate the endocannabinoid system indirectly, as CBD does by preventing anandamide degradation (Bisogno et al, 2001; Izzo et al, 2009), would seem to be more advantageous than using cannabinoid type-1 receptor agonists to do so because of the abuse potential of the latter compounds (Steckler and Risbrough, 2012).
In summary, the present findings provide compelling evidence for a disruptive effect of CBD on recent and older contextual fear memories by the blockade of their reconsolidation, resulting in a long lasting attenuation of freezing. Importantly, this effect of cannabidiol is time-specific and dependent on both memory reactivation and on activation of cannabinoid type-1 receptors. Our findings encourage further studies aiming at investigating the clinical potential of this compound to uncouple/reduce the negative valence associated with emotional memories when given either alone or combined with psychological interventions.
References
Akirav I, Khatsrinov V, Vouimba RM, Merhav M, Ferreira G, Rosenblum K et al (2006). Extinction of conditioned taste aversion depends on functional protein synthesis but not on NMDA receptor activation in the ventromedial prefrontal cortex. Learn Mem 13: 254–258.
Akirav I, Maroun M (2006). Ventromedial prefrontal cortex is obligatory for consolidation and reconsolidation of object recognition memory. Cerebral Cortex 16: 1759–1765.
Alberini CM (2011). The role of reconsolidation and the dynamic process of long-term memory formation and storage. Front Behav Neurosci 7: 5–12.
Bhattacharyya S, Fusar-Poli P, Borgwardt S, Martin-Santos R, Nosarti C, O'Carroll C et al (2009). Modulation of mediotemporal and ventrostriatal function in humans by Delta9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry 66: 442–451.
Bergamaschi MM, Queiroz RH, Chagas MH, de Oliveira DC, De Martinis BS, Kapczinski F et al (2011). Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naïve social phobia patients. Neuropsychopharmacology 36: 1219–1226.
Bisogno T, Hanus L, De Petrocellis L, Tchilibon S, Ponde DE, Brandi I et al (2001). Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol 134: 845–852.
Bitencourt RM, Pamplona FA, Takahashi RN (2008). Facilitation of contextual fear memory extinction and anti-anxiogenic effects of AM404 and cannabidiol in conditioned rats. Eur Neuropsychopharmacol 18: 849–859.
Blanchard RJ, Blanchard DC (1969). Passive and active reactions to fear-eliciting stimuli. J Comp Physiol Psychol 68: 129–135.
Boccia MM, Blake MG, Krawczyk MC, Baratti CM (2011). Sildenafil, a selective phosphodiesterase type 5 inhibitor, enhances memory reconsolidation of an inhibitory avoidance task in mice. Behav Brain Res 220: 319–324.
Bustos SG, Giachero M, Maldonado H, Molina VA (2010). Previous stress attenuates the susceptibility to midazolam's disruptive effect on fear memory reconsolidation: influence of pre-reactivation D-cycloserine administration. Neuropsychopharmacology 35: 1097–1108.
Bustos SG, Maldonado H, Molina VA (2006). Midazolam disrupts fear memory reconsolidation. Neuroscience 139: 831–842.
Bustos SG, Maldonado H, Molina VA (2009). Disruptive effect of midazolam on fear memory reconsolidation: decisive influence of reactivation time span and memory age. Neuropsychopharmacology 34: 446–457.
Campos AC, Guimarães FS (2008). Involvement of 5HT1A receptors in the anxiolytic-like effects of cannabidiol injected into the dorsolateral periaqueductal gray of rats. Psychopharmacology (Berl) 199: 223–230.
Casarotto PC, Gomes FV, Resstel LB, Guimarães FS (2010). Cannabidiol inhibitory effect on marble-burying behaviour: involvement of CB1 receptors. Behav Pharmacol 21: 353–358.
de Oliveira Alvares L, Pasqualini Genro B, Diehl F, Molina VA, Quillfeldt JA (2008). Opposite action of hippocampal CB1 receptors in memory reconsolidation and extinction. Neuroscience 154: 1648–1655.
Debiec J, Doyère V, Nader K, Ledoux JE (2006). Directly reactivated, but not indirectly reactivated, memories undergo reconsolidation in the amygdala. Proc Natl Acad Sci USA 103: 3428–3433.
Debiec J, Ledoux JE (2004). Disruption of reconsolidation but not consolidation of auditory fear conditioning by noradrenergic blockade in the amygdala. Neuroscience 129: 267–272.
Debiec J, LeDoux JE, Nader K (2002). Cellular and systems reconsolidation in the hippocampus. Neuron 36: 527–538.
Deiana S, Watanabe A, Yamasaki Y, Amada N, Arthur M, Fleming S et al (2012). Psychopharmacology (Berl) 219: 859–873.
Dudai Y (2004). The neurobiology of consolidations, or, how stable is the engram? Annu Rev Psychol 55: 51–86.
Dudai Y (2006). Reconsolidation: the advantage of being refocused. Curr Opin Neurobiol 16: 174–178.
Duvarci S, Nader K (2004). Characterization of fear memory reconsolidation. J Neurosci 24: 9269–9275.
Duvarci S, Nader K, LeDoux JE (2005). Activation of extracellular signal-regulated kinase- mitogen-activated protein kinase cascade in the amygdala is required for memory reconsolidation of auditory fear conditioning. Eur J Neurosci 21: 283–289.
Eisenberg M, Kobilo T, Berman DE, Dudai Y (2003). Stability of retrieved memory: inverse correlation with trace dominance. Science 301: 1102–1104.
Fanselow MS (2010). From contextual fear to a dynamic view of memory systems. Trends Cogn Sci 14: 7–15.
Gatley SJ, Gifford AN, Volkow ND, Lan R, Makriyannis A (1996). 123I-labeled AM251: a radioiodinated ligand which binds in vivo to mouse brain cannabinoid CB1 receptors. Eur J Pharmacol 307: 331–338.
Guimarães FS, Chiaretti TM, Graeff FG, Zuardi AW (1990). Antianxiety effect of cannabidiol in the elevated plus-maze. Psychopharmacology (Berl) 100: 558–559.
Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR et al (1990). Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA 87: 1932–1936.
Herry C, Trifilieff P, Micheau J, Lüthi A, Mons N (2006). Extinction of auditory fear conditioning requires MAPK/ERK activation in the basolateral amygdala. Eur J Neurosci 24: 261–269.
Izzo AA, Borrelli F, Capasso R, Di Marzo V, Mechoulam R (2009). Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci 30: 515–527.
Kobilo T, Hazvi S, Dudai Y (2007). Role of cortical cannabinoid CB1 receptor in conditioned taste aversion memory. Eur J Neurosci 25: 3417–3421.
Lattal KM, Abel T (2004). Behavioral impairments caused by injections of the protein synthesis inhibitor anisomycin after contextual retrieval reverse with time. Proc Natl Acad Sci USA 101: 4667–4672.
Lee JL (2010). Memory reconsolidation mediates the updating of hippocampal memory content. Front Behav Neurosci 4: 168.
Lee JL, Everitt BJ, Thomas KL (2004). Independent cellular processes for hippocampal memory consolidation and reconsolidation. Science 304: 839–843.
Lee JL, Milton AL, Everitt BJ (2006). Reconsolidation and extinction of conditioned fear: inhibition and potentiation. J Neurosci 26: 10051–10056.
Lin HC, Mao SC, Gean PW (2006). Effects of intra-amygdala infusion of CB1 receptor agonists on the reconsolidation of fear-potentiated startle. Learn Mem 13: 316–321.
Milekic MH, Alberini CM (2002). Temporally graded requirement for protein synthesis following memory reactivation. Neuron 36: 521–525.
Misanin JR, Miller RR, Lewis DJ (1968). Retrograde amnesia produced by electroconvulsive shock after reactivation of a consolidated memory trace. Science 160: 554–555.
Moreira FA, Aguiar DC, Guimarães FS (2006). Anxiolytic-like effect of cannabidiol in the rat Vogel conflict test. Prog Neuropsychopharmacol Biol Psychiatry 30: 1466–1471.
Mueller D, Porter JT, Quirk GJ (2008). Noradrenergic signaling in infralimbic cortex increases cell excitability and strengthens memory for fear extinction. J Neurosci 28: 369–375.
Nader K, Schafe GE, Le Doux JE (2000). Fear memories require protein synthesis in the amygdala for reconsolidation after retrieval. Nature 406: 722–726.
Nurmikko TJ, Serpell MG, Hoggart B, Toomey PJ, Morlion BJ, Haines D (2007). Sativex successfully treats neuropathic pain characterised by allodynia: a randomised, double-blind, placebo-controlled clinical trial. Pain 133: 210–220.
Ogren SO, Eriksson TM, Elvander-Tottie E, D'Addario C, Ekström JC, Svenningsson P et al (2008). The role of 5-HT(1A) receptors in learning and memory. Behav Brain Res 195: 54–77.
Pike VW, Halldin C, McCarron JA, Lundkvist C, Hirani E, Olsson H et al (1998). [carbonyl-11C]Desmethyl-WAY-100635 (DWAY) is a potent and selective radioligand for central 5-HT1A receptors in vitro and in vivo. Eur J Nucl Med 25: 338–346.
Przybyslawski J, Roullet P, Sara SJ (1999). Attenuation of emotional and nonemotional memories after their reactivation: role of beta adrenergic receptors. J Neurosci 19: 6623–6628.
Rescorla RA (2004). Spontaneous recovery varies inversely with the training-extinction interval. Learn Behav 32: 401–408.
Resstel LB, Tavares RF, Lisboa SF, Joca SR, Corrêa FM, Guimarães FS (2009). 5-HT1A receptors are involved in the cannabidiol-induced attenuation of behavioural and cardiovascular responses to acute restraint stress in rats. Br J Pharmacol 156: 181–188.
Rodriguez-Ortiz CJ, Garcia-DeLaTorre P, Benavidez E, Ballesteros MA, Bermudez-Rattoni F (2008). Intrahippocampal anisomycin infusions disrupt previously consolidated spatial memory only when memory is updated. Neurobiol Learn Mem 89: 352–359.
Russo EB, Burnett A, Hall B, Parker KK (2005). Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res 30: 1037–1043.
Sara SJ (2000). Retrieval and reconsolidation: toward a neurobiology of remembering. Learn Mem 7: 73–84.
Schafe GE, LeDoux JE (2000). Memory consolidation of auditory pavlovian fear conditioning requires protein synthesis and protein kinase A in the amygdala. J Neurosci 20: RC96.
Steckler T, Risbrough V (2012). Pharmacological treatment of PTSD – established and new approaches. Neuropharmacology 62: 617–627.
Suzuki A, Josselyn SA, Frankland PW, Masushige S, Silva AJ, Kida S (2004). Memory reconsolidation and extinction have distinct temporal and biochemical signatures. J Neurosci 24: 4787–4795.
Suzuki A, Mukawa T, Tsukagoshi A, Frankland PW, Kida S (2008). Activation of LVGCCs and CB1 receptors required for destabilization of reactivated contextual fear memories. Learn Mem 15: 426–433.
Taubenfeld SM, Riceberg JS, New AS, Alberini CM (2009). Preclinical assessment for selectively disrupting a traumatic memory via postretrieval inhibition of glucocorticoid receptors. Biol Psychiatry 65: 249–257.
Yamada D, Zushida K, Wada K, Sekiguchi M (2009). Pharmacological discrimination of extinction and reconsolidation of contextual fear memory by a potentiator of AMPA receptors. Neuropsychopharmacology 34: 2574–2584.
Yehuda R, Joëls M, Morris RG (2010). The memory paradox. Nat Rev Neurosci 11: 837–839.
Acknowledgements
This work was supported by Brazilian grants from Fundação de Amparo à Pesquisa do Estado de São Paulo (07/03685-3), and Conselho Nacional de Desenvolvimento Científico e Tecnológico (308457/2008-0, 480903/2010-7). We thank the anonymous reviewers and Professor G A Rae for constructive comments on the manuscript, as well as Professor J M Neto for kindly donating the WAY100635.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Stern, C., Gazarini, L., Takahashi, R. et al. On Disruption of Fear Memory by Reconsolidation Blockade: Evidence from Cannabidiol Treatment. Neuropsychopharmacol 37, 2132–2142 (2012). https://doi.org/10.1038/npp.2012.63
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.63
Keywords
This article is cited by
-
Evidence on the impairing effects of Ayahuasca on fear memory reconsolidation
Psychopharmacology (2022)
-
Effects of cannabidiol on symptoms induced by the recall of traumatic events in patients with posttraumatic stress disorder
Psychopharmacology (2022)
-
Comparison between cannabidiol and sertraline for the modulation of post-traumatic stress disorder-like behaviors and fear memory in mice
Psychopharmacology (2022)
-
Effects of Cannabis on PTSD Recovery: Review of the Literature and Clinical Insights
Current Addiction Reports (2022)
-
Effects of ∆9-tetrahydrocannabinol on aversive memories and anxiety: a review from human studies
BMC Psychiatry (2020)