Abstract
The need for safer, more effective therapeutics for the treatment of schizophrenia is widely acknowledged. To optimally target novel pharmacotherapies, in addition to establishing the mechanisms responsible for the beneficial effects of antipsychotics, the pathways underlying the most severe side effects must also be elucidated. Here we investigate the role of serotonin 2A (5-HT2A), serotonin 2C (5-HT2C), and dopamine 2 receptors (D2) in mediating adverse effects associated with canonical first- and second-generation antipsychotic drugs in mice. Wild-type (WT) and 5-HT2A knockout (KO) mice treated with haloperidol, clozapine, and risperidone were assessed for locomotor activity and catalepsy. WT mice showed a marked reduction in locomotor activity following acute administration of haloperidol and high-dose risperidone, which was most likely secondary to the severe catalepsy caused by these compounds. Clozapine also dramatically reduced locomotor activity, but in the absence of catalepsy. Interestingly, 5-HT2A KO mice were cataleptic following haloperidol and risperidone, but did not respond to clozapine's locomotor-suppressing effects. Restoration of 5-HT2A expression to cortical glutamatergic neurons re-instated the locomotor-suppressing effects of clozapine in the open field. In sum, we confirm that haloperidol and risperidone caused catalepsy in rodents, driven by strong antagonism of D2. We also demonstrate that clozapine decreases locomotor activity in a 5-HT2A-dependent manner, in the absence of catalepsy. Moreover, we show that it is the cortical population of 5-HT2A that mediate the locomotor-suppressing effects of clozapine.
Similar content being viewed by others
INTRODUCTION
Schizophrenia is characterized by profound disruptions in thinking, affect, language, perception, and sense of self. This impacts upon normal functioning through impaired capacity to earn a livelihood, and while some patients respond well to currently available antipsychotic drugs, others remain symptomatic. Findings from the CATIE study (Lieberman et al, 2005) revealed that up to 74% of patients prescribed atypical antipsychotics discontinued treatment as a result of either ineffectiveness of the antipsychotic or intolerability of the side effects, which include sedation, cardiometabolic risks, extrapyramidal symptoms (EPS), agranulocytosis, and cognitive dulling (Leucht et al, 2009).
Clozapine—the prototypical atypical antipsychotic—remains one of the most efficacious antipsychotics available (McEvoy et al, 2006; Meltzer et al, 2003). Clozapine has been shown to bind upwards of 50 receptor targets in vitro (Roth et al, 2004) showing strong affinity for dopaminergic, serotonergic, muscarinic, adrenergic, and histaminergic receptors; however, the full spectrum of its in vivo receptor affinity is subject to some discussion (Beninger et al, 2010; Coward, 1992; McCormick et al, 2010; Roth et al, 2004; Schotte et al, 1993). Although it pioneered second-generation drugs, which have lower liability to cause EPS and tardive dyskinesias, these compounds are hampered by side effects such as weight gain, hyperlipidemia, agranulocytosis, and sedation. The severity of these side effects is such that clozapine is prescribed for treatment only as a last resort. A better understanding of how clozapine and other atypical antipsychotics produce both therapeutic and unwanted effects remains a field of active investigation.
The most popular explanation for the improved efficacy in treating negative symptoms and the low EPS produced by atypical antipsychotic compounds is the addition of strong serotonin 2A receptor (5-HT2A) antagonism. Antagonism of 5-HT2A in mesocortical pathways is hypothesized to be one of the mechanisms underlying the improvement of negative symptoms produced by atypical antipsychotics, whereas the attenuated EPS have been proposed to be the result of 5-HT2A antagonist-driven dopamine release in the striatum (Meltzer and Massey, 2011). However, studies investigating these hypotheses have provided mixed results in both humans and mice, and alternative hypotheses have been proposed to explain the reduction in EPS, including an anti-cholinergic mechanism or the action of α2-adrenoceptor antagonism (Kalkman et al, 1998a, 1998b; Parada et al, 1997).
To shed light upon the manner by which atypical antipsychotics circumvent the induction of EPS, we used a combined pharmacological and genetic strategy. If the prevailing hypotheses held true, then administering haloperidol either in combination with a 5-HT2A antagonist or to a 5-HT2A knockout mouse (KO) should shift the phenotype from catalepsy/EPS to something more closely resembling the effects of atypical antipsychotics. Moreover, using a STOP-floxed 5-HT2A transgenic mouse, we should be able to pinpoint the neural loci controlling this behavioral shift.
Contrary to our hypothesis, we found that 5-HT2A signaling alone does not appear to be critical to the shift away from EPS in second-generation drugs. Interestingly, we found that the receptor plays a key role in the regulation of locomotor suppression produced by atypical antipsychotics, like clozapine, and that this response relied upon the expression of 5-HT2A specifically in the forebrain.
MATERIALS AND METHODS
Animals
Animals were housed on a 12 h light/dark cycle with food and water available ad libitum. All testing was carried out during the light cycle on 5-HT2A KO mice and wild-type (WT) littermate controls on a 129SvEv/Tac background originally obtained from Taconic (Taconic Farms). Mice heterozygous for a transgenic STOP cassette flanked by LoxP sites located upstream of the htr2a gene (Weisstaub et al, 2006) were crossed, generating WT, KO, and heterozygous littermates, identified by PCR genotyping. Mice were weaned at 3–4 weeks of age and behavioral testing began at 12 weeks.
Restricted expression of specific populations of 5-HT2A was achieved as described previously. Briefly, STOP-floxed htr2a transgenic mice were crossed with mice expressing Emx1-Cre to selectively express 5-HT2A in Emx1-positive cells (predominantly pyramidal forebrain neurons as has been demonstrated previously; Weisstaub et al, 2006). A DAT-Cre mouse line was used to selectively restore 5-HT2A expression to DAT-containing nigrostriatal neurons.
Drugs
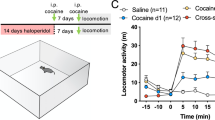
Antipsychotics were tested at a range of doses (Figure 1) before selecting a single dose for subsequent testing: clozapine (5 mg/kg), haloperidol (0.4 mg/kg), risperidone (0.4 mg/kg), AC90179 (10 mg/kg), which shows high potency as an inverse agonist and a competitive antagonist at the 5-HT2A, and SB242084 (1 mg/kg), a 5-HT2C inverse agonist with some activity at the 5-HT2B receptor or vehicle (1% Tween-80 at pH 6.0).
Mice were treated with antipsychotic drugs across a range of doses and locomotor activity in the open field was assessed for 30 min. Haloperidol, at doses of 0.1 mg/kg and higher, significantly decreased locomotor activity in both wild-type (WT) and serotonin 2A (5-HT2A) knockout (KO) mice (a: untreated, N=26 WT, 34 KO; haloperidol treated, N=11 KO, 9 WT). Risperidone at both low and high doses also decreased activity comparably in both WT and KO mice (b: untreated, N=26 WT, 34 KO; haloperidol treated, N=11 KO, 9 WT). Clozapine treatment resulted in extreme sedation in WT mice from 5 mk/kg upwards (c: untreated, N=26 WT, 34 KO; haloperidol treated, N=12 KO, 8 WT). In KO mice, clozapine did not induce this extreme level of sedation until 30 mg/kg. Data are shown as mean±SEM. #P<0.05 difference from WT.
Locomotor Activity
Animals were treated intraperitoneally 30 min before being placed in the MedAssociates locomotor arena, and were then tracked for 30 min using the MedAssociates software. Diphenhydramine displayed a shorter window of efficacy on behavior. As a result, mice were placed in the locomotor arena immediately following drug administration.
Catalepsy Assessment
Catalepsy was assessed using the step down task. Step down task was performed by placing the forepaws or hindpaws on a bar 0.8 cm in diameter fixed at 3.5 cm from the bench top. Mice were injected intraperitoneally 30 min before testing. Time to step down was measured for three consecutive trials for an average step down time.
Neurological Reflex/Motor Behavior
Righting reflex was assessed using a subjective scoring matrix. A score of 0 was allocated to mice that righted immediately (too quickly to time accurately), 1 for animals that turned noticeably more slowly (righted in approximately 1 s), a score of 2 was given to animals that displayed great difficulty in turning over (righted in 1+ s), and a score of 3 indicated mice that did not right at all.
RESULTS
Dose Response to Haloperidol, Risperidone, and Clozapine
Clozapine, haloperidol, and risperidone display distinct pharmacology. Haloperidol, a typical antipsychotic, demonstrates highest affinity for the D2 receptor and σ1 receptor, robustly antagonizing signaling at relatively low doses (Roth et al, 2004; Schotte et al, 1996). Risperidone possesses a broader spectrum, showing high in vitro affinity for 5-HT2A, 5-HT7, D2, α1, and H1, and is reported to act like an atypical antipsychotic at lower doses, but more like a typical antipsychotic at higher doses (Roth et al, 2004; Schotte et al, 1996). Clozapine has a complex pharmacology, binding to upwards of 50 receptors with demonstrable affinity for 5-HT2A, 5-HT2C, D2, H1, and M1 receptors (Roth et al, 2004; Schotte et al, 1996; Yadav et al, 2011).
Haloperidol dramatically reduced activity across both genotypes (Figure 1a: effect of treatment, F(7,224)=28.706, P<0.0001; effect of genotype, F(1,224)=0.465, P=0.4958; genotype × treatment interaction, F(7,224)=0.338, P=0.9359). A significant effect of genotype was detected in the risperidone dose–response curve in addition to the treatment effect; however, the genotypes were not differentially affected by the treatment (Figure 1b: effect of treatment, F(7,224)=21.972, P<0.0001; effect of genotype, F(1,224)=4.065, P<0.05; genotype × treatment interaction, F(7,224)=0.084, P=0.9990). Clozapine affected WT and 5-HT2A KO mice differentially (Figure 1c: effect of treatment, F(7,224)=13.169, P<0.0001; effect of genotype, F(1,224)=22.166, P<0.0001; genotype × treatment interaction, F(7,224)=2.698, P<0.05): decreasing mice locomotor activity in WT mice in a dose dependent manner. 5-HT2A KO displayed a U-shaped dose–response curve, which may be attributable to the increased 5-HT2C antagonism at higher doses of clozapine.
From these dose–response curves, a dose of 5 mg/kg was chosen for clozapine, 0.4 mg/kg for haloperidol, and 0.4 mg/kg for risperidone.
Antipsychotic-Induced Catalepsy Occurs Independently of 5HT2A Receptors
Typical antipsychotics provoke a cataleptic response in mice, which is considered to be analogous to EPS in human patients. This response is widely attributed to the robust antagonism of D2 receptors in both mice and humans; however, it has also been suggested to be susceptible to modulation by 5-HT2A.
No significant effect of 5-HT2A genotype was observed in the dose–response analysis of catalepsy (Figure 2a: haloperidol—effect of treatment, F(7,704)=235.118, P<0.0001; effect of genotype, F(1,2.513)=0.465, P=0.1134; risperidone—effect of treatment, F(7,704)=169.293, P<0.0001; effect of genotype, F(1,704)=0.001, P=0.9737).
Haloperidol and risperidone caused catalepsy in both wild-type (WT) (N=19–33) and knockout (KO) mice (N=21–31) in a dose-dependent manner (a). At doses of 0.4 mg/kg haloperidol and risperidone both induced catalepsy relative to vehicle-treated mice. Clozapine 5 mg/kg (N=22 WT, 19 KO), however, did not induce catalepsy in either genotype (b). The serotonin 2A (5-HT2A) antagonist AC90179 (c) (N=21 WT, 23 KO) and the 5-HT2C antagonist SB242084 (d) (N=34 WT, 30 KO) alone did not affect catalepsy nor did they alter the cataleptic response to haloperidol (N=9–13). Mice treated with risperidone and SB242084 (N=11 WT, 10 KO) showed significantly less catalepsy than haloperidol-treated mice (e: N=10 WT, 12 KO). They were also significantly different to mice treated with vehicle (N=10 WT, 9 KO) (e). Co-administration of SB242084 and AC90179 with haloperidol (N=10 WT, 11 KO) also attenuated catalepsy. However, catalepsy levels were still significantly higher than vehicle-treated mice (N=10 WT, 9 KO) (e). Data are shown as mean±SEM. ***P<0.0001 difference from vehicle treatment.
With the selected doses of antipsychotics, a significant statistical effect of treatment was observed in response to antipsychotic drugs (Figure 2b: ANOVA effect of genotype, F(1,260)=0.338, P=0.5614; effect of treatment, F(3,260)=102.44, P<0.0001). Haloperidol and risperidone induced catalepsy on the step down task (Figure 2b: haloperidol compared with vehicle-treated animals, P<0.0001; risperidone vs vehicle, P<0.0001). Clozapine did not cause catalepsy in mice (P=0.4815) nor did the administration of AC90179 (Figure 2c: effect of genotype, F(1, 243)=1.108, P=0.2935; effect of treatment, F(3,243)=116.673, P<0.0001; AC90179 vs vehicle, P=0.2082) or SB242084 (Figure 2d: effect of genotype, F(1,265)=0.101, P=0.7509; effect of treatment, F(3,265)=124.749, P<0.0001; SB242084 vs vehicle, P=0.2126). Interestingly, while ‘risperidone with SB242084’ and ‘haloperidol with AC90179 and SB242084’ both induced significant catalepsy relative to vehicle-treated mice (Figure 2e: effect of genotype, F(1,243)=0.2224, P=0.2224; effect of treatment, F(3,243)=66.491, P<0.0001; risperidone+SB242084 vs vehicle, P<0.0001; haloperidol+AC90179+SB242084 vs vehicle, P<0.0001), they were nonetheless significantly less cataleptic than haloperidol alone (risperidone+SB242084 vs haloperidol, P<0.0001; haloperidol+AC90179+SB242084 vs haloperidol, P<0.0001).
5HT2A KO Mice Show Altered Locomotor Response to Clozapine, but not Risperidone or Haloperidol
Antipsychotic treatment significantly reduced locomotor activity (Figure 3a: effect of treatment, F(3, 71)=10.841, P<0.0001). There was also a significant overall effect of 5-HT2A genotype (F(1, 71)=12.231, P<0.001) and an interaction (F(3, 71)=10.841, P<0.001). Post hoc analyses revealed that in WT mice, haloperidol (P<0.0001), risperidone (P<0.0001), and clozapine (P<0.01) all caused significant reduction of locomotor activity (Figure 3a).
Clozapine, risperidone, and haloperidol reduced locomotor activity in wild-type (WT) mice (N=10 per treatment), relative to vehicle-treated animals (N=9) (a). Serotonin 2A (5-HT2A) knockout (KO) mice were sensitive to the locomotor suppression caused by haloperidol (N=10) and risperidone (N=10), but were resistant to the effects of clozapine (N=10) (a). AC90179 alone was not significantly different from vehicle (b) (N=10 per group) and SB242084 increased activity in both genotypes (N=10 per group). Co-administration resulted in a significant increase in activity in KO mice (N=13, P<0.05), while in WT mice AC90179 antagonism of the 5-HT2A cancelled out the hyperlocomotion produced following SB242084 alone (N=9) (b). Mice treated with haloperidol and AC90179 (N=10 per group) were significantly different from vehicle, but not from haloperidol alone (c). Mice treated with SB242084 (N=10 per group) again displayed hyperactivity relative to vehicle-treated mice (N=11 per group) (d). Haloperidol (N=10 WT, 12 KO) decreased distance traveled, while haloperidol plus SB242084 (N=13 WT, 9 KO) was significantly different from haloperidol alone (P<0.0001) and from SB242084 alone (P<0.0001), but not from vehicle treatment (P<0.6860) (d). A significant effect of genotype was seen following clozapine administration (N=12 WT, 9 KO; vehicle-treated mice, N=10 WT, 9 KO). Significant differences were also observed following risperidone+SB242084 (N=21 WT, 22 KO) and a trend was observed following co-injection of haloperidol, AC90179, and SB242084 (N=10 WT, 11 KO) (treatment effect, P=0.071; genotype effect, P<0.1085) (e). Data are shown as mean±SEM. *P<0.05, **P<0.01, ***P<0.0001 difference from vehicle treatment. #P<0.05, ###P<0.0001 indicates a significant difference in behavior of the KO relative to WT mice under the same treatment regimen.
Haloperidol and risperidone decreased activity equally in both WT and 5-HT2A KO mice. This is most likely a corollary of the catalepsy induced by these drugs at the doses used. Clozapine, in the absence of catalepsy-like behavior, showed a gene × treatment interaction (F(1, 35)=8.386, P<0.01): 5-HT2A KO mice were resistant to the locomotor suppression produced by clozapine (Figure 3a: P<0.01 compared to WT mice).
The 5-HT2C receptor antagonist SB242084 significantly increased locomotor activity (Figure 3b: effect of treatment, F(3, 78)=18.865, P<0.0001; effect of genotype, F(1, 78)=9.865, P<0.01; SB242084 vs vehicle, P<0.0001; AC90179 vs vehicle, P=0.7613). In 5-HT2A KO mice, co-administration of AC90179 and SB242084 produced the same increased activity observed following SB242084 alone (P<0.05). In WT mice, the combined antagonism of the 5-HT2A and 5-HT2C resulted in no significant differences from vehicle-treated mice (P=0.4052) indicative of a counterbalancing effect of 5-HT2A and 5-HT2C antagonism on locomotor activity.
Combined D2 and 5-HT2A antagonism caused significant locomotor suppression, independent of genotype, an effect that was similar to that of haloperidol alone (Figure 3c: effect of treatment, F(3, 75)=39.284, P<0.0001; effect of genotype, F(1,75)=1.898, P=0.1724; haloperidol+AC90179 vs haloperidol, P=0.9647; haloperidol+AC90179 vs risperidone, P=0.8570), and was significantly different to vehicle treatment (P<0.0001). Interestingly, SB242084 administered in combination with haloperidol resulted in a significant reduction in locomotor activity compared to SB242084 alone (Figure 3d: effect of treatment, F(3,78)=17.584, P<0.0001; effect of genotype, F(1,78)=0.145, P=0.7042; haloperidol+SB242084 vs SB242084, P<0.001), but not significantly different from vehicle (P=0.6860) nor haloperidol alone (P=0.1103; Figure 3d).
The genotype effect of clozapine administration could be recapitulated by treating mice with risperidone (which shares clozapine's affinity at the D2 and 5-HT2A) in combination with SB242084 (Figure 3e: effect of treatment, F(3,74)=2.002, P=0.121; effect of genotype, F(1,74)=7.569, P<0.01; treatment × genotype interaction, F(3,74)=1.473, P=0.2288). WT mice display locomotor suppression comparable to clozapine alone (risperidone+SB242084 vs clozapine, P=0.8255), which was significantly different from their baseline activity (P<0.01), whereas 5-HT2A KO mice, following risperidone and SB242084, were not different from vehicle treatment (P=0.7472) or clozapine treatment (P=0.3536). This was also achievable by the combination of haloperidol, AC90179, and SB242084, which in WT mice was significantly different from vehicle treatment (P<0.05), but not clozapine treatment (P=0.3290), while in 5-HT2A KO mice there was no difference between this combination of drugs and vehicle (P=0.6210), or clozapine (P=0.8972).
Thus, clozapine suppresses locomotor activity in a 5-HT2A-dependent manner, in the absence of catalepsy, suggesting an alternate mechanism.
Differential Response to Atypical Antipsychotics in 5-HT2A KO Mice is not due to Changes in Histaminergic or Muscarinic Signaling
To determine the involvement of 5-HT2C in mediating locomotor suppression induced by clozapine, 5-HT2C knockout mice were treated with either saline or clozapine and assessed in the open field. WT and 5-HT2C KO mice displayed comparable levels of locomotor suppression following 5 mg/kg clozapine treatment (Figure 4a: treatment effect, F(1,29)=15.146, P<0.001; genotype effect, F(1,29)=0.003, P=0.9564).
Wild-type (WT) mice and serotonin 2C (5-HT2C) knockout (KO) mice showed comparable levels of baseline locomotion and were equally affected by clozapine treatment of 5 mg/kg (a). In 5-HT2A KO mice, olanzapine produces a similar effect to that observed following clozapine, with WT mice demonstrating reduced locomotor behavior relative to saline-treated animals, while 5HT2A KO mice are resistant to this effect (b). Scopolamine (c) and diphenhydramine (d) both produced an increase in locomotion that was not dependent on 5-HT2A receptor signaling. Data are shown as mean±SEM. **P<0.01, ***P<0.0001 difference from vehicle treatment. ###P<0.0001 indicates a significant difference in behavior of the KO relative to WT mice under the same treatment regimen.
Moreover the behavioral response to clozapine was found to generalize to other, similar atypical antipsychotics. Olanzapine dramatically reduced locomotion (Figure 4b: effect of treatment, F(1,33)=12.671, P<0.01; effect of genotype, F(1,33)=2.031, P=0.1635; genotype × treatment interaction, F(1,33)=4.979, P<0.05), an effect that was again observed to be muted in 5-HT2A KO mice (P<0.0001).
Given clozapine's affinity for M1 and H1, and the possible interactions between these receptors and the 5-HT2A (Hirano et al, 1995; Morisset et al, 1999), locomotor response to muscarinic and histaminergic antagonism were assessed to test the hypothesis that the differential response to atypical antipsychotics may be a product of alterations in these neurotransmitter systems.
Mice showed robust locomotor activation following scopolamine treatment (1 mg/kg) independent of their genotype (Figure 4c: effect of treatment, F(1,36)=73.721, P<0.0001; effect of genotype, F(1,36)=0.290, P=0.5937). Diphenhydramine (6 mg/kg) also increased locomotor activity equally in both WT and 5-HT2A KO mice (effect of treatment, F(1,36)=8.899, P<0.01; effect of genotype, F(1,36)=0.011, P=0.9176).
Forebrain Glutamatergic 5HT2A is Sufficient to Recapitulate the WT-Like Response to Atypical Antipsychotics
Transgenic animals with 5-HT2A selectively expressed in restricted neural regions were generated as described previously (Weisstaub et al, 2006). The Emx1 lineage of cells includes cortical and hippocampal glutamatergic neurons in addition to subpopulations of oligodendrocytes and astrocytes (Gorski et al, 2002; Guo et al, 2000), whereas the DAT-Cre results in strong recombination in the VTA and SNc, in addition to weak expression in the olfactory bulb and the hypothalamus (Zhuang et al, 2005).
Locomotor activity
Emx1-Cre: As observed previously, we found an overall effect of genotype (F(3,50)=4.233, P<0.01; Figure 5a) and treatment (F(1, 50)=28.888, P<0.0001), as well as an interaction (F(3,50)=3.125, P<0.05). Clozapine severely reduced locomotor activity relative to saline treatment in WT and Cre control animals (P<0.01 for WT and P<0.001 for Cre control; Figure 5a). 5-HT2A KO mice were not susceptible to the locomotor-suppressing effects of clozapine, showing no significant differences compared with their KO saline-treated littermates (P=0.9503). 5-HT2A expression in forebrain glutamatergic neurons alone was sufficient to restore the locomotor-suppressing effects of clozapine (P<0.01; Figure 5a).
As found previously, clozapine dramatically reduced locomotor activity in wild-type (WT) mice (a) (N=7) as well as in Cre control mice (N=8). The locomotor behavior of serotonin 2A (5-HT2A) knockout (KO) mice was unaffected by clozapine treatment (N=7); however, mice expressing htr2ar in the cortex (N=7 saline, 8 clozapine treated) behaved like WT mice, showing decreased locomotor activity following clozapine treatment. (b) At baseline, 5-HT2A-DAT-Cre rescue mice showed slightly elevated baseline activity. Clozapine attenuated this locomotion in WT and DAT-Cre control mice; however, it did not affect the activity of KO (n=11) or 5HT2A-DAT mice (N=15). (c) Clozapine impaired the righting reflex in WT mice (N=7) and EMX1-Cre control mice (N=8). Righting reflex was not impaired in KO mice following clozapine (N=7) nor was it impaired in 5-HT2A-EMX1-Cre mice (N=7). (d) In a subsequent cohort of mice, we again observed impaired righting reflex in WT (n=15) and DAT-Cre control mice (N=12). KO mice were resistant to this response (N=11) as were 5-HT2A-DAT-Cre rescue mice (N=15). No significant genotype effects were observed in saline-treated mice as none of the groups displayed impaired righting reflex (data not shown). Data are shown as mean±SEM. **P<0.01, ***P<0.0001 difference from vehicle treatment. #P<0.05, ##P<0.01, ###P<0.0001 indicates a significant difference in behavior of the KO relative to WT mice under the same treatment regimen.
DAT-Cre: Given the important role of dopamine in motor behavior and the high expression of 5-HT2A on dopamine neurons, we had hypothesized that antagonism of this population of 5-HT2A might be responsible for clozapine's cataleptic effects. We again observed an effect of genotype (F(3, 99)=8.667, P<0.0001) and a genotype × treatment interaction (F(3, 99)=2.998, P<0.05); however, expression of 5-HT2A in DAT-Cre-expressing neurons did not restore clozapine's locomotor-suppressing effect (Figure 5b: KO vs DAT-Cre-driven 5-HT2A-expressing mice, P=0.1068).
Righting reflex
Another measure of sedative behavior is the righting reflex. We measured the righting reflex in WT, Cre controls, 5-HT2A KO mice, and mice with 5HT2A expressed in either Emx1 or DAT cell lineages (Figures 5c and d), following clozapine or saline administration.
EMX1-Cre: A. significant effect of treatment was observed (F(1, 50)=23.747, P<0.0001; Figure 5c) with clozapine exerting a sedative effect on the mice. This effect was not equal across all genotypes with significant genotype (F(3, 50)=5.662, P<0.01) and genotype × treatment interaction (F(3, 50)=5.662, P<0.01) effects observed. The interaction was caused by significant differences in response to clozapine, where 5-HT2A KO mice were not observed to be sedated following clozapine (KO vs WT, P<0.01; KO vs Cre control, P<0.01). Moreover, the rescue of 5HT2A in the cortex did not restore WT-like behavior to the mice (Rescue vs WT, P<0.05; Rescue vs Cre control, P<0.05; Rescue vs KO, P=0.5698).
DAT-Cre: Expression of 5-HT2A in nigrostriatal neurons did not restore the locomotor-suppressing effects of clozapine (Figure 5d). Again a significant effect of treatment (F(1, 99)=59.515, P<0.0001), genotype (F(3, 99)=25.126, P<0.0001), and a treatment × genotype interaction (F(3, 99)=25.872, P<0.0001) was observed. 5-HT2A KO mice and mice with 5-HT2A expressed only in DAT-containing cells were significantly different to WT mice (P<0.0001 and P<0.0001, respectively) and to Cre control mice (P<0.0001 and P<0.0001, respectively). DAT-Cre 5-HT2A mice did not differ significantly from 5-HT2A KO mice (P=0.5192).
DISCUSSION
Advances in psychopharmacotherapy have seen an increase in efficacy and decreased EPS, but second-generation antipsychotics are nonetheless associated with unpleasant side effects. Although these compounds are highly non-selective, research using animal models is helping to unravel the role of specific receptors in the beneficial effects and the adverse effects. Recent studies demonstrate that 5-HT2A antagonists can attenuate psychotomimetic behavioral responses, by modulating serotonergic tone (Martin et al, 1998). That said, it has also been shown that while modulation of the serotonergic tone is necessary for the therapeutic effects of clozapine (Yadav et al, 2011), this is not dependent on either 5-HT2A (predominantly postsynaptic) (Yadav et al, 2011) or 5HT1A (largely autoreceptors) (Scorza et al, 2010). In this context, the central role played by 5-HT2A in mediating the adverse effects of atypical antipsychotics acquires increased significance for future drug discovery.
The focus of this study was the behavioral response to combined D2, 5-HT2A, and 5-HT2C receptor antagonism, common to many atypical antipsychotics and several interesting findings emerge. Primarily, we show that atypical antipsychotic-induced locomotor suppression is driven by a forebrain glutamatergic locus of activity, and that 5-HT2A receptors mediate this effect. The data also support the role of D2 in mediating catalepsy in mice, and appear to preclude a role for 5-HT2A receptors in controlling this response. Finally, these experiments reproduce the oppositional relationship between 5-HT2A and 5-HT2C in their influence over locomotor behavior (Halberstadt et al, 2009).
The Role Played by 5-HT2AR in Catalepsy
Catalepsy in rodents is considered to accurately predict EPS in humans and both behaviors are thought to result from strong antagonism at the D2. Although some studies have implicated serotonin in the modulation of cataleptic behavior, reports have been mixed, and a rationale for the divergence in these findings has not been proposed. A catalepsy-prone strain of inbred rats display decreased 5-HT2A in the striatum in comparison to the catalepsy-resistant Wistar rat strain (Kulikov et al, 2002). Furthermore, the combined 5-HT2A/5-HT2C antagonist, ketanserin, has been postulated to overcome the cataleptic effects of haloperidol (Creed-Carson et al, 2011). However, a separate study demonstrated that lower doses of a 5-HT2A inverse agonist did not affect cataleptic behavior following either haloperidol or risperidone (Gardell et al, 2007). Interestingly, both agonism (Prinssen et al, 2002) and antagonism (Wadenberg, 1996) of the 5-HT1A have been shown to weaken catalepsy in rodents, whereas the antagonists have been shown to attenuate EPS in primates (Casey, 1993).
Consistent with published work, we show that haloperidol and high-dose risperidone cause catalepsy in rodents, driven by strong antagonism at the D2 (seen in many first-generation neuroleptics as well as high doses of some second-generation antipsychotics, such as risperidone) (Wiley and Evans, 2008). In support of the findings of Gardell and colleagues, in our dose–response curve we show that WT mice are no more sensitive to catalepsy than 5-HT2A KO mice following haloperidol and risperidone. Nonetheless, we do report some attenuation of the catalepsy response in mice treated with haloperidol in combination with both 5-HT2A and 5-HT2C antagonists, whereas neither of these compounds affected haloperidol-induced catalepsy on their own. Taken together, our findings, and those reported previously, suggest that substantial changes in serotonergic signaling through multiple receptors are required to overcome the catalepsy caused by D2 antagonism following typical antipsychotic administration. This may be achieved either by targeting the presynaptic 5-HT1A, controlling 5-HT release and thus the postsynaptic response, or by directly blocking both postsynaptic 5-HT2 receptors. This supports the notion that the primary and most crucial mechanism underlying neuroleptic-induced catalepsy is via the indirect striatopallidal output pathway, driven by D2 blockade.
Serotonergic Control of Locomotor Activation and Suppression
Locomotor suppression induced by clozapine in rodents is widely acknowledged; however, there has been a paucity of research invested in addressing the mechanism by which this is achieved. The results herein provide critical insight into how these behaviors occur; however, the unexpected nature of the findings also open up several important avenues for further investigation. How does 5-HT2Aregulate these behaviors? Which second messenger systems control this response? Can we dissociate these pathways from those that control therapeutic efficacy?
Inverse agonism of 5-HT2A and 5-HT2C (with AC90179 and SB242084 respectively), administered in combination with haloperidol, resulted in reduced locomotor activity, similar to that observed following atypical antipsychotics. Although it is not possible to definitively relate the atypical antipsychotic-induced locomotor suppression directly to a human correlate, it is tempting to speculate that the decreased activity in mice may be analogous to the sedative effects of atypical antipsychotics in schizophrenia patients. Muscarinic M1 receptors, histaminergic H1 receptors, and α1 adrenergic receptors (Cooper, 1986; Nicholson, 1983; Sallinen et al, 2007) have been associated with wakefulness and their respective neurotransmitters are known to be involved in the arousal pathways (Castberg et al, 2006; Stahl, 2008; Stahl and Shayegan, 2003). As such, the belief has been that these receptors and their downstream signaling systems are likely to be responsible for atypical antipsychotic-induced sedation, which has a significant impact on the quality of life of schizophrenia patients (Asenjo Lobos et al, 2010). In addition, previous reports have shown that blocking dopamine D2 can cause locomotor suppression and neurolepsis at high doses (Huang et al, 2010; Shireen and Haleem, 2011; Starr and Starr, 1987); however, this is likely associated with the cataleptic nature of D2 antagonism.
Here, we show that 5-HT2A receptors are required to produce this phenotype. To our knowledge, 5-HT2A has not previously been considered as a target for this behavior. As such, it is important to note that 5-HT2A have been shown to influence H1 and M1 signaling (Hirano et al, 1995; Morisset et al, 1999). However, although we cannot rule it out altogether, our results are indicative of a locomotor suppression that is independent of histaminergic or muscarinic tone, as we do not observe a differential response to diphenhydramine, a histamine receptor antagonist, nor to scopolamine, a muscarinic antagonist, in the 5-HT2A knockout mice, relative to WT mice.
Interestingly, while WT mice display a dose-dependent decrease in locomotor behavior in response to clozapine, 5-HT2A KO mice display a muted, U-shaped, locomotor response curve, which may be attributable to the yin–yang relationship between 5-HT2A and 5-HT2C. The data show that antagonism of 5-HT2C produces robust locomotor activation that can be attenuated by antagonism of the 5-HT2A receptor, findings that complement previously published research demonstrating that agonism at the 5-HT2A increases activity in a manner which can be countered by 5-HT2C agonism (Halberstadt et al, 2009). With increasing doses of clozapine one would produce increasing antagonism at the 5HT2C, resulting in locomotor activation in the absence of 5-HT2A receptors.
We also observed a divergence in the population of 5-HT2A responsible for locomotor suppression vs the righting reflex, which may be attributed to subtle differences in the behaviors being tested, the level of motivation required to perform the task, and the underlying neural circuits. In fact, while we demonstrate the importance of cortical 5-HT2A in mediating locomotor suppression, it is generally believed that the righting reflex is predominantly a cerebellar behavior (Johnson et al, 1985; Spuhler et al, 1982; Tanaka and Okeda, 2000).
Another interesting finding, which may provide some clue as to the underlying mechanism, is the distinction between the effects of chronic absence of the 5-HT2A and the effect of acute antagonism of this receptor. Specifically, that clozapine (a 5-HT2A antagonist) is dependent on the presence of the 5-HT2A, but not 5-HT2C, for its locomotor-suppressing effects is seemingly counter-intuitive. In this context, it is important to consider how the constitutive absence of 5-HT2A might impact upon neural development, and adult neurochemistry and neuroanatomy. To date, we have not identified any significant compensatory changes caused by the constitutive absence of 5HT2A that could explain the observed genotype difference (Weisstaub et al, 2006). That said, more thorough investigations may reveal additional changes in other signaling pathway components. One such possibility would be changes in expression of the immediate early gene (IEG), Egr3. The potential importance of Egr3 in mediating this behavior, and its possible link to the 5-HT2A receptor, is presented in detail in a recent publication and we will thus refrain from further elaboration on the relevance of this point (Williams et al, 2012; Gallitano-Mendel et al, 2008). However, should this signaling pathway be found to modulate 5-HT2A activity, it would provide a parsimonious explanation for the divergence between the effect of the receptor knockout and the pharmacological inactivation of the receptor. Moreover, it would be consistent with the decreased expression of 5-HT2A observed in the egr3 KO mice.
Conclusions
To date, the neurochemical and neuroanatomical loci underlying many of the side effects associated with clozapine have not been widely explored and academic discourse and drug discovery have moved forward in the absence of this important information. This series of experiments are among the first to identify categorically a neural locus for the locomotor suppression induced by clozapine, while at the same time identifying a novel target for the neurochemical pathways involved (see also Williams et al, 2012). The regulation of clozapine-induced locomotor suppression by glutamatergic forebrain 5-HT2A-expressing neurons provides insight into the adverse effects of antipsychotics, clarifying our understanding of the neural circuitry underlying the side effects induced by antipsychotics.
References
Asenjo Lobos C, Komossa K, Rummel-Kluge C, Hunger H, Schmid F, Schwarz S et al (2010) Clozapine vs other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev: CD006633.
Beninger RJ, Baker TW, Florczynski MM, Banasikowski TJ (2010). Regional differences in the action of antipsychotic drugs: implications for cognitive effects in schizophrenic patients. Neurotox Res 18: 229–243.
Casey DE (1993). Serotonergic and dopaminergic aspects of neuroleptic-induced extrapyramidal syndromes in nonhuman primates. Psychopharmacology (Berl) 112 (Suppl): S55–S59.
Castberg I, Reimers A, Sandvik P, Aamo TO, Spigset O (2006). Adverse drug reactions of antidepressants and antipsychotics: experience, knowledge and attitudes among Norwegian psychiatrists. Nord J Psychiatry 60: 227–233.
Cooper Jr JW (1986). H-1 blockers—classical antihistamines. N Engl Reg Allergy Proc 7: 356–361.
Coward DM (1992). General pharmacology of clozapine. Br J Psychiatry Suppl 17: 5–11.
Creed-Carson M, Oraha A, Nobrega JN (2011). Effects of 5-HT(2A) and 5-HT(2C) receptor antagonists on acute and chronic dyskinetic effects induced by haloperidol in rats. Behav Brain Res 219: 273–279.
Gallitano-Mendel A, Wozniak DF, Pehek EA, Milbrandt J (2008). Mice lacking the immediate early gene Egr3 respond to the anti-aggressive effects of clozapine yet are relatively resistant to its sedating effects. Neuropsychopharmacology 33: 1266–1275.
Gardell LR, Vanover KE, Pounds L, Johnson RW, Barido R, Anderson GT et al (2007). ACP-103, a 5-hydroxytryptamine 2A receptor inverse agonist, improves the antipsychotic efficacy and side-effect profile of haloperidol and risperidone in experimental models. J Pharmacol Exp Ther 322: 862–870.
Gorski JA, Talley T, Qiu M, Puelles L, Rubenstein JL, Jones KR (2002). Cortical excitatory neurons and glia, but not GABAergic neurons, are produced in the Emx1-expressing lineage. J Neurosci 22: 6309–6314.
Guo H, Hong S, Jin XL, Chen RS, Avasthi PP, Tu YT et al (2000). Specificity and efficiency of Cre-mediated recombination in Emx1-Cre knock-in mice. Biochem Biophys Res Commun 273: 661–665.
Halberstadt AL, van der Heijden I, Ruderman MA, Risbrough VB, Gingrich JA, Geyer MA et al (2009). 5-HT(2A) and 5-HT(2C) receptors exert opposing effects on locomotor activity in mice. Neuropsychopharmacology 34: 1958–1967.
Hirano H, Day J, Fibiger HC (1995). Serotonergic regulation of acetylcholine release in rat frontal cortex. J Neurochem 65: 1139–1145.
Huang AC, Shyu BC, Hsiao S (2010). Dose-dependent dissociable effects of haloperidol on locomotion, appetitive responses, and consummatory behavior in water-deprived rats. Pharmacol Biochem Behav 95: 285–291.
Johnson SW, Hoffer BJ, Baker R, Freedman R (1985). Correlation of Purkinje neuron depression and hypnotic effects of ethanol in inbred strains of rats. Alcohol Clin Exp Res 9: 56–58.
Kalkman HO, Neumann V, Hoyer D, Tricklebank MD (1998a). The role of alpha2-adrenoceptor antagonism in the anti-cataleptic properties of the atypical neuroleptic agent, clozapine, in the rat. Br J Pharmacol 124: 1550–1556.
Kalkman HO, Neumann V, Nozulak J, Tricklebank MD (1998b). Cataleptogenic effect of subtype selective 5-HT receptor antagonists in the rat. Eur J Pharmacol 343: 201–207.
Kulikov AV, Barykina NN, Tikhonova MA, Chuguy VF, Kolpakov VG, Popova NK (2002). Effect of chronic thyroxine treatment on catalepsy in rats. Neurosci Lett 330: 207–209.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM (2009). Second-generation vs first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 373: 31–41.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO et al (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 353: 1209–1223.
Martin P, Waters N, Schmidt CJ, Carlsson A, Carlsson ML (1998). Rodent data and general hypothesis: antipsychotic action exerted through 5-Ht2A receptor antagonism is dependent on increased serotonergic tone. J Neural Transm 105: 365–396.
McCormick PN, Kapur S, Graff-Guerrero A, Raymond R, Nobrega JN, Wilson AA (2010). The antipsychotics olanzapine, risperidone, clozapine, and haloperidol are D2-selective ex vivo but not in vitro. Neuropsychopharmacology 35: 1826–1835.
McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA et al (2006). Effectiveness of clozapine vs olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry 163: 600–610.
Meltzer H, Massey B (2011). The role of serotonin receptors in the action of atypical antipsychotic drugs. Curr Opin Pharmacol 11: 59–67.
Meltzer HY, Perry E, Jayathilake K (2003). Clozapine-induced weight gain predicts improvement in psychopathology. Schizophr Res 59: 19–27.
Morisset S, Sahm UG, Traiffort E, Tardivel-Lacombe J, Arrang JM, Schwartz JC (1999). Atypical neuroleptics enhance histamine turnover in brain via 5-hydroxytryptamine2A receptor blockade. J Pharmacol Exp Ther 288: 590–596.
Nicholson AN (1983). Antihistamines and sedation. Lancet 2: 211–212.
Parada MA, Hernandez L, Puig de Parada M, Rada P, Murzi E (1997). Selective action of acute systemic clozapine on acetylcholine release in the rat prefrontal cortex by reference to the nucleus accumbens and striatum. J Pharmacol Exp Ther 281: 582–588.
Prinssen EP, Colpaert FC, Koek W (2002). 5-HT1A receptor activation and anti-cataleptic effects: high-efficacy agonists maximally inhibit haloperidol-induced catalepsy. Eur J Pharmacol 453: 217–221.
Roth BL, Sheffler DJ, Kroeze WK (2004). Magic shotguns vs magic bullets: selectively non-selective drugs for mood disorders and schizophrenia. Nat Rev Drug Discov 3: 353–359.
Sallinen J, Hoglund I, Engstrom M, Lehtimaki J, Virtanen R, Sirvio J et al (2007). Pharmacological characterization and CNS effects of a novel highly selective alpha2C-adrenoceptor antagonist JP-1302. Br J Pharmacol 150: 391–402.
Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS et al (1996). Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 124: 57–73.
Schotte A, Janssen PF, Megens AA, Leysen JE (1993). Occupancy of central neurotransmitter receptors by risperidone, clozapine and haloperidol, measured ex vivo by quantitative autoradiography. Brain Res 631: 191–202.
Scorza MC, Castane A, Bortolozzi A, Artigas F (2010). Clozapine does not require 5-HT1A receptors to block the locomotor hyperactivity induced by MK-801 Clz and MK-801 in KO1A mice. Neuropharmacology 59: 112–120.
Shireen E, Haleem DJ (2011). Reversal of haloperidol-induced motor deficits by mianserin and mesulergine in rats. Pak J Pharm Sci 24: 7–12.
Spuhler K, Hoffer B, Weiner N, Palmer M (1982). Evidence for genetic correlation of hypnotic effects and cerebellar Purkinje neuron depression in response to ethanol in mice. Pharmacol Biochem Behav 17: 569–578.
Stahl SM (2008). Antipsychotics and Mood Stabilizers 3rd edn. Cambridge University Press.
Stahl SM, Shayegan DK (2003). The psychopharmacology of ziprasidone: receptor-binding properties and real-world psychiatric practice. J Clin Psychiatry 64 (Suppl 19): 6–12.
Starr BS, Starr MS (1987). Behavioural interactions involving D1 and D2 dopamine receptors in non-habituated mice. Neuropharmacology 26: 613–619.
Tanaka G, Okeda R (2000). N-[4-(3-ethoxy-2-hydropropoxy)phenyl] acrylamide selectively induces apoptosis of cerebellar granule cells in vivo and in vitro in rats. Acta Neuropathol 99: 337–344.
Wadenberg ML (1996). Serotonergic mechanisms in neuroleptic-induced catalepsy in the rat. Neurosci Biobehav Rev 20: 325–339.
Weisstaub NV, Zhou M, Lira A, Lambe E, Gonzalez-Maeso J, Hornung JP et al (2006). Cortical 5-HT2A receptor signaling modulates anxiety-like behaviors in mice. Science 313: 536–540.
Wiley JL, Evans RL (2008). Evaluation of age and sex differences in locomotion and catalepsy during repeated administration of haloperidol and clozapine in adolescent and adult rats. Pharmacol Res 58: 240–246.
Williams AA, Ingram WM, Levine S, Resnik J, Kamel CM, Lish JR et al (2012). Reduced levels of serotonin 2A receptors underline resistance of Egr 3 deficient mice to locomotor suppression by clozapine. Neuropsychopharmacology; e-pub ahead of print 13 June 2012.
Yadav PN, Abbas AI, Farrell MS, Setola V, Sciaky N, Huang XP et al (2011). The presynaptic component of the serotonergic system is required for clozapine's efficacy. Neuropsychopharmacology 36: 638–651.
Zhuang X, Masson J, Gingrich JA, Rayport S, Hen R (2005). Targeted gene expression in dopamine and serotonin neurons of the mouse brain. J Neurosci Methods 143: 27–32.
Acknowledgements
We acknowledge Acadia Pharmaceuticals for the generous gift of the AC90179. We would also like to acknowledge funding from the NH&MRC (CEM), NIMH, NIDA (5 PO1 DA012923-08), Lieber Center for Schizophrenia Research, and the Sackler Institute (JAG). We thank Elena Demireva, Elizabeth LaMarca, and Maria Milekic for their vital input to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
McOmish, C., Lira, A., Hanks, J. et al. Clozapine-Induced Locomotor Suppression is Mediated by 5-HT2A Receptors in the Forebrain. Neuropsychopharmacol 37, 2747–2755 (2012). https://doi.org/10.1038/npp.2012.139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.139
Keywords
This article is cited by
-
Clozapine N-oxide, compound 21, and JHU37160 do not influence effortful reward-seeking behavior in mice
Psychopharmacology (2024)
-
Effect of 5-HT2A receptor antagonism on levels of D2/3 receptor occupancy and adverse behavioral side-effects induced by haloperidol: a SPECT imaging study in the rat
Translational Psychiatry (2021)
-
Revealing the structure of pharmacobehavioral space through motion sequencing
Nature Neuroscience (2020)
-
Role of mGlu2 in the 5-HT2A receptor-dependent antipsychotic activity of clozapine in mice
Psychopharmacology (2018)
-
Effect of clozapine on ketamine-induced deficits in attentional set shift task in mice
Psychopharmacology (2017)