Abstract
Impairments in attention are a major component of the cognitive symptoms of neuropsychiatric and neurodegenerative disorders. Using an operant sustained attention task (SAT), including a distractor condition (dSAT), we assessed the putative pro-attentional effects of the selective α4β2* nicotinic acetylcholine receptor (nAChR) agonist S 38232 in comparison with the non-selective agonist nicotine. Neither drug benefited SAT performance. However, in interaction with the increased task demands implemented by distractor presentation, the selective agonist, but not nicotine, enhanced the detection of signals during the post-distractor recovery period. This effect is consistent with the hypothesis that second-long increases in cholinergic activity (‘transients’) mediate the detection of cues and that nAChR agonists augment such transients. Electrochemical recordings of prefrontal cholinergic transients evoked by S 38232 and nicotine indicated that the α4β2* nAChR agonist evoked cholinergic transients that were characterized by a faster rise time and more rapid decay than those evoked by nicotine. Blockade of the α7 nAChR ‘sharpens’ nicotine-evoked transients; therefore, we determined the effects of co-administration of nicotine and the α7 nAChR antagonist methyllycaconitine on dSAT performance. Compared with vehicle and nicotine alone, this combined treatment significantly enhanced the detection of signals. These results indicate that compared with nicotine, α4β2* nAChR agonists significantly enhance attentional performance and that the dSAT represents a useful behavioral screening tool. The combined behavioral and electrochemical evidence supports the hypothesis that nAChR agonist-evoked cholinergic transients, which are characterized by rapid rise time and fast decay, predict robust drug-induced enhancement of attentional performance.
Similar content being viewed by others
INTRODUCTION
Efforts to discover and develop treatments for the cognitive symptoms of neuropsychiatric and neurodegenerative disorders have been hampered by the absence of effective ‘benchmark’ drugs and preclinical screening and characterization procedures that reliably predict clinical efficacy of putative cognition enhancers. Furthermore, theories that would define promising neuropsychopharmacological target mechanisms for the development of cognition enhancers have remained rare (eg Hagan and Jones, 2005; Sarter, 2006).
Attentional functions and capacities are key variables of cognitive performance (Sarter et al, 2005, 2006), and as such have been extensively targeted for drug-induced cognition enhancement. Cholinergic activity is necessary for the performance of attention tasks (eg McGaughy et al, 1996; for review see Sarter et al, 2005, 2006). The development of enzyme-coated microelectrodes allowing for the amperometric monitoring of real-time acetylcholine (ACh) release has revealed that brief (on the scale of seconds) increases in cholinergic activity (henceforth termed ‘transients’) mediate the detection of cues in attentional contexts (Parikh et al, 2007). This finding explains the exclusive impairment in the ability to report the presence of a signal observed after cholinergic lesions, whereas non-signal trial-response accuracy remains completely spared (McGaughy et al, 1996).
Agonists at nicotinic acetylcholine receptors (nAChRs), particularly the non-selective agonist nicotine, have been extensively shown to benefit attention in healthy human beings, patient groups, as well as in intact animals and animal models (eg Newhouse et al, 2004; Sahakian et al, 1989; Levin et al, 1998; Hahn et al, 2003; Sarter, 2010). However, the magnitude of the effects of nicotine was often relatively small and depended on individual task demands and parameters, treatment regimen, and subjects’ prior exposure to nicotine (Manusco et al, 1999; Mirza and Stolerman, 1998; Rusted et al, 2000; Mirza and Bright, 2001; Hahn et al, 2002; Bizarro and Stolerman, 2003). Moreover, effects were restricted to secondary measures of performance (Blondel et al, 2000), did not reach significance (Turchi et al, 1995), or even indicated impaired performance (Bushnell et al, 1997). In recent years, agonists or positive allosteric modulators of nAChR subtypes have been developed based in part on the expectation that such compounds exhibit greater pro-attentional efficacy when compared with nicotine (eg Prendergast et al, 1998; McGaughy et al, 1999; Potter et al, 1999; Wilens et al, 1999, 2006; Grottick and Higgins, 2000; Lippiello et al, 2006; Dunbar et al, 2007; Wilens and Decker, 2007).
Local administration of α4β2* nAChR agonists evokes abrupt increases in cholinergic activity within the cortex that mirror, specifically in terms of rise time, amplitude, and decay rate, the ‘sharp’ transients observed in task-performing animals (Parikh et al, 2008). In contrast, nicotine generates long-lasting release events (up to and over 1 min) that are partly mediated through stimulation of the α7 nAChR (Parikh et al, 2008, 2010). On the basis of these and additional results, we hypothesized that α4β2* nAChR agonists more robustly enhance attentional performance than nicotine, as the long release event evoked by nicotine may limit its ability to enhance trial-based performance in tasks involving cholinergically mediated cognitive operations occurring on much shorter timescales (Sarter et al, 2009a).
The first aim of this study was to compare the effects of S 38232, a selective, full agonist at α4β2* nAChRs (Lagostena et al, 2010), with the effects of the non-selective agonist nicotine on the performance of rats in the distractor version of the sustained attention task (dSAT). This task was originally developed for research in animals and has been cross-validated for research in human beings (Demeter et al, 2008; Nuechterlein et al, 2009; see Supplementary Figure S1). Post-distractor performance recovery is thought to be mediated, top down, through activation of prefrontal networks (Weissman et al, 2004; Johnston et al, 2007). As high demands on cognitive performance are a major determinant of showing attentional benefits of nicotine in healthy subjects (Newhouse et al, 2004), dSAT performance was expected to reveal such effects. The second aim of this study was to determine the characteristics of cholinergic transients evoked by S 38232 and nicotine. Third, we tested the hypothesis that co-administration of nicotine and the α7 nAChR antagonist methyllycaconitine (MLA) results in greater pro-attentional effects than nicotine administered alone, owing to the ‘sharpening’ of nicotine-evoked transients by α7 nAChR blockade.
MATERIALS AND METHODS
Subjects
For the behavioral experiments, subjects were male Wistar rats (Harlan, IN) ∼200–300 g at the onset of training. Animals were kept on a 14 : 10 light/dark cycle in a temperature and humidity-controlled vivarium. Water was available only as a reward during testing and for 30 min on the completion of a training/testing session. Food was available ad libitum. All training and testing took place during the light cycle. Subjects used for electrochemical studies were adult male Fisher/Brown Norway hybrid rats (FBNF1; Harlan, IN) ∼200–250 g at the beginning of the experiments. Food and water was available ad libitum. All animals were maintained in accordance with the NIH guide for the Care and Use of Animals, and experiments were conducted in accordance with protocols approved by the University of Michigan Committee on Use and Care of Animals.
SAT Acquisition and Performance Criteria
The SAT (Figure S1 in Supplementary data; see also Kozak et al, 2006, 2007) is comprised of a series of randomly presented signal (500–25 ms illumination of a central panel light) and non-signal events. After a signal or non-signal event, two retractable levers are extended into the operant chamber, prompting animals to report the presence or absence of a signal. The task generates four measures of performance (Supplementary Figure S1): hits (H) and misses (M) are correct and incorrect responses on signal trials, respectively; correct rejections (CR) and false alarms (FA) are correct and incorrect responses on non-signal trials, respectively. A houselight is left on throughout the task. Final performance criterion was defined as >70% hits to 500 ms signals and >70% CR for three consecutive sessions. After reaching the criterion level, animals continued daily practice sessions and were habituated for 1 week to systemic injections (i.p.) of saline.
Assessment of Performance During the dSAT
As illustrated in Supplementary Figure S1, in the dSAT, the first 8-min block of trials (block 1) was identical to the SAT described above. This block was followed by a 16-min block (block 2) with the distractor (chamber houselight flashing on/off at 0.5 Hz) turned on. After distractor termination, performance recovery was determined during a final 16-min block of the regular SAT (block 3). Animals practiced the dSAT a minimum of two times before the effects of S 38232 and nicotine on performance were tested. Individual distractor test sessions were separated by a minimum of 2 days of SAT practice sessions, with performance at or above the criterion level. Our evidence indicates that repeated exposure to the distractor does not significantly alter the efficacy of the distractor, including the rate of post-distractor performance recovery.
Measures of SAT and dSAT Performance
Data from both SAT and dSAT test sessions were grouped into three blocks of trials for analysis: the first 8 min of task performance (block 1), the second 16 min of task performance (block 2), and the final 16 min of task performance (block 3). For each session, the total number H and M by signal duration, CR, FA, and omissions were recorded. Using these values, the relative number of hits (h=H/(H+M)), CR (cr=CR/(FA+CR)), misses (1−h), and FA (1-cr) were determined. Scores were calculated for each block of trials, signal duration, as well as averaged across signal durations.
Drugs, Drug Administration, and Doses
S 38232 (N-{[1-(methylamino)cyclopropyl]methyl}-3-pyridinamine) was obtained from Institut de Recherches Internationales Servier (Courbevoie, France). The compound is a full agonist at α4β2* nAChRs, with an EC50 of 3.4 × 10−6 M to rat α4β2* nAChRs expressed in Xenopus laevis oocytes. Furthermore, the compound has a low partial agonist activity at rat α7 nAChR (EC50 of 1.3 × 10−4 M; Servier, unpublished data; Lagostena et al, 2010). Nicotine (nicotine hydrogene tartrate; Sigma-Aldrich, St Louis, MO) and S 38232 were administered to separate groups of animals. SAT performance was determined after administration of S 38232 (n=11; 0.03, 0.30, 1.00, and 3.00 mg/kg) or nicotine (n=14; 0.02, 0.10, 0.40 mg/kg; base weights). Both compounds were dissolved in sterile saline. Animals were given a systemic injection (i.p.) and placed into the operant chambers for the duration of a pre-task wait period (15 min for nicotine, 30 min for S 38232). The administration of doses and vehicle was randomized for each animal. Successive administrations of drug doses were separated by a minimum of 2 days/sessions in which the animal's SAT performance was at or above criterion level. Vehicle was administered before all other test sessions. The selection of doses for dSAT testing was based on the effects on SAT performance and, therefore, is explained in Results. Finally, we tested the effects of nicotine (0.1 mg/kg) administered together with the α7 nAChR antagonist MLA citrate hydrate (MLA; Sigma-Aldrich; n=9; 1.0 or 5.0 mg/kg; 1 ml/kg for all injections; 15 min before task onset; see Blondel et al, 2000). All compounds were dissolved in sterile saline. The pH of the solutions (7.4–7.6) was adjusted using sodium hydroxide solution. These effects were determined in animals that also received nicotine alone before a dSAT performance test to allow for within-subjects comparisons.
Electrochemical Recordings of nAChR Agonist-Evoked Cholinergic Transients In Vivo
Details concerning the preparation and calibration of choline-sensitive microelectrodes are described in Supplementary data (see also Parikh et al, 2007, 2008). Briefly, cholinergic transients were measured using ceramic-based choline-selective microelectrodes and fixed-potential amperometry (Quanteon, Nicholasville, KY). Each electrode was equipped with four platinum recording sites arranged in side by side pairs. Choline oxidase (CHOase) was cross-linked with a bovine serum albumin (BSA)/glutaradehyde solution, and immobilized on the bottom pair of recording sites. The other pair was coated with the BSA/glutaraldehyde solution alone and served to record fluctuations in the background current. Meta-phenylenediamine was electropolymerized onto the surface of the recording sites to block electroactive interferents. Electrodes were calibrated in vitro (see Table 1 in Supplementary data). Animals were anesthetized with urethane (1.25–1.5 g/kg; i.p.) and placed in a stereotaxic frame. Body temperature was maintained at 37°C with an isothermal pad. Single barrel glass capillaries (1.0 × 0.58 mm, 6 in.; A-M systems, Carlsborg, WA) were pulled using a micropipette puller (Model # 51210, Stoelting, Wood Dale, IL). Micropipettes (inner tip diameter ∼15 μm) were attached to the microelectrode with the tip centered between the two pairs of recording sites, ∼70 μm from the surface of the electrode. The assembly was positioned in either the right or left medial prefrontal cortex (AP: +3.0 mm, ML±0.7 mm, DV: −3.0 mm from bregma). A Ag/AgCl reference wire was implanted in the opposite hemisphere, and a fixed potential of +0.7 V was held between the reference and recording electrodes. Amperometric recordings were made at 1 Hz, and data was digitized using a FAST-16 recording system (Quanteon LLC, Nicholasville, KY). Experiments began after stabilization of baseline current (45–60 min). Drug solutions were pressure ejected through the micropipettes, and ejection volumes were monitored through a stereoscope equipped with a reticule.
S 38232 was delivered through intracranial pressure ejections of 200 nl of drug solution (40 pmol, n=5; 200 pmol, n=6, and 2 nmol, n=5). Cholinergic transients evoked by S 38232 were compared with those evoked by nicotine (the data on nicotine, including the effect of MLA on nicotine-evoked transients were taken from Parikh et al, 2008). In addition, the effects of dihydro-β-erythoidine (DHβE), a relatively selective α4β2* nAChR antagonist, on signals evoked by S 38232 were assessed. DHβE (Tocris Bioscience; Ellisville, MO) was infused (1.6 nmol in 800 nl over 5 s) and was followed 3 min later by a series of three pressure ejections of S 38232 (2 nmol, n=5).
Current recordings on CHOase-coated channels were self-referenced as described in Parikh et al (2008). Transients evoked by S 38232 or nicotine were compared with respect to peak amplitudes and signal decay rate (t50; time required for the signal to decline by 50% of peak amplitude). Data from three cholinergic signals per drug manipulation and per animal were averaged and used for statistical analysis.
Statistical Methods
Performance was analyzed using repeated-measures ANOVAs with dose of drug, performance block, and signal duration as within-subjects factors. Mixed model ANOVAs with the between-subjects factor of group were used to show that baseline performance did not differ between animals treated with nicotine or S 38232. One-way ANOVAs with dose as a between-subjects variable were used to determine dose–response relationships and to compare evoked cholinergic transients evoked by the two nAChR agonists. All post hoc analyses used the least significant differenced test (LSD). When necessary, main effects and interactions were further investigated with independent and paired samples t-tests (α=0.05). Exact p-values were reported as suggested by Greenwald et al (1996). Furthermore, the results from repeated-measures ANOVAs indicate uncorrected degrees of freedom, but Huynh–Feldt-corrected F-values.
RESULTS
Baseline SAT Performance
Baseline SAT performance did not differ between animals used to test the effects of nicotine and S 38232. As shown in Figure 1a, the relative number of hits declined with decreasing signal duration (F(2,46)=184.09; p<0.001). Animals correctly rejected 88.80±1.40% (M; SEM) of non-signal events (Figure 1b). SAT performance did not vary across the three blocks of trials, and the effects of block did not interact with group and/or signal duration (all p>0.25). Finally, animals omitted few trials (0.88±0.26% of ∼200 trials/session) and the number of omissions did not differ between the groups (p=0.40).
Baseline SAT performance and effects of S 38232 and nicotine on SAT performance: (a) depicts baseline hit rate as a function of signal duration and (b) shows the correct rejection rate of the three blocks of trials. Baseline performance did not differ between groups that were treated with nicotine or S 38232, respectively. Administration of the highest dose of nicotine decreased the number of hits to longest signals (c). All doses of nicotine decreased the correct rejection rate in block 1 (e). Administration of S 38232 did not affect hits (d). A small decrease in the relative number of correct rejections in block 2 was caused by the highest dose (f). The main effects of signal duration are indicated in (c) and (d). (For this and subsequent figures: *p<0.05, **p<0.01; ***p<0.001; based on multiple comparisons conducted on the basis of significant results of ANOVA; see Results.).
Neither Nicotine nor S 38232 Enhance SAT Performance
Administration of the non-selective nAChR agonist nicotine (0.02, 0.1, 0.4 mg/kg) did not enhance SAT performance (dose: F(3,39)=1.31; p=0.28). Rather, as illustrated in Figure 1c, the highest dose of nicotine produced a small, but robust decrease in the hit rate to longest signals (dose × signal: F(6,78)=5.50; p<0.001; see figures for post hoc comparisons). Furthermore, all three doses of nicotine resulted in a decrease in the relative number of CR during block 1. These effects were not seen during subsequent blocks of trials (dose: F(3,39)=5.63; p=0.013; dose × block: F(6,78)=6.42; p<0.001; Figure 1e). Finally, the highest dose of nicotine also increased the number of omitted trials (F(3,39)=8.05; p=0.014), from 0.66±0.29% after vehicle to 12.29±4.07% after the administration of 0.4 mg/kg. Furthermore, the increase in omissions was highest during the first block of trials (main effect of block: F(2,26)=4.69; p=0.043; dose by block: F(6,78)=4.51; p=0.046).
Administration of S 38232 (0.03, 0.3, 1.0, and 3.0 mg/kg) did not affect the animals’ hit rate (Figure 1d; all main effects and interactions including dose: all p>0.10). However, the highest dose of S 38232 resulted in a small yet significant decrease in the relative number of CR during the second block of trials (Figure 1f; dose: F(4,40)=0.84; p=0.49; dose × block: (F(8,80)=2.31; p=0.03). The number of omitted trials increased over blocks of trials (F(2,20)=5.30; p=0.02), from 1.46±0.66% in block 1 to 2.26±0.65% in block 3; however, this increase was not affected by the administration of S 38232 (F(8,80)=1.90; p=0.15).
Taken together, neither the administration of the selective α4β2* nAChR agonist nor the non-selective agonist nicotine benefited the performance of the standard SAT. The impairments caused by either drug were small and/or remained limited to a particular block of trials.
Distractor-Induced Impairment and Performance Recovery
The dSAT baseline (vehicle) performance did not differ between animals scheduled to be treated with S 38232 or nicotine (all main effects of group and interactions involving group: p>0.20). As illustrated in Figure 2a and b, presentation of the distractor resulted in robust decreases in both the relative number of hits and CR. Concerning hits, the effect of block interacted significantly with signal duration (block: (F(2,46)=23.66; p<0.001; block × signal: F(4,92)=16.21; p<0.001). Post hoc comparisons (illustrated in Figure 2a) indicated an acute decrease in hits during the distractor block and a partial but incomplete recovery of the hit rate to longest signals during the post-distractor block. In contrast, hits to medium duration signals did not recover and hits to shortest signals were lower during the post-distractor block than during both preceding blocks of trials. In contrast, the distractor-induced decrease in CR recovered completely during block 3 (main effect of block: (F(2,46)=73.62; p<0.001; Figure 2b).
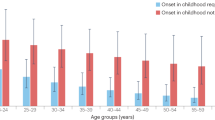
Characterization of the effects of distractor presentation on performance: (a) depicts the relative number of hits for all three signal durations and across the three blocks of trials. Note that the hit rate to longest, but not to shortest, signals recovered partly during the post-distractor block of trials. In contrast, correct rejections recovered completely (b). (c) Administration of S 38232 significantly benefited the hit rate during the post-distractor block of trials. As shown in (d), the administration of nicotine did not affect dSAT performance. In contrast, co-administration of nicotine and MLA enhanced the hit rate in all three blocks of trials (e). Although (d) suggests that the beneficial effects of this co-treatment were most pronounced during the post-distractor block of trials, ANOVA indicated that the effects of treatment and block did not interact significantly. *p<0.05; **p<0.01; ***p<0.001.
Enhancement of dSAT Performance by S 38232
On the basis of the detrimental effect of the highest dose of S 38233 on SAT performance (see above), and inspection of (insignificant) effects of dose on all measures of SAT performance, a dose of 0.3 mg/kg was selected for dSAT testing. In the analysis of effects on dSAT performance, putative drug effects were expected to interact with the factor ‘block,’ reflecting that drug effects would manifest in the presence of, or subsequent to, distractor presentation. Such an interaction was found with respect to hits (Figure 2c; F(2,20)=6.86; p=0.006).
As would be expected, based on the effects of this dose of S 38232 on SAT performance (above), post hoc comparisons did not indicate an effect of S 38232 on hits obtained from the pre-distractor block 1. Likewise, S 38232 did not affect the low number of hits during the presence of the distractor in block 2. However, S 38232 enhanced the hits rate during the post-distractor block 3 (F(1,10)=7.09; p=0.024; Figure 2c).
Nicotine Did Not Affect dSAT Performance
As illustrated in Figure 1c, the highest dose of nicotine impaired the detection of longest signals in animals performing the SAT (above). Therefore, the next highest dose was selected for dSAT testing (0.1 mg/kg; see also Hahn et al, 2002). This dose of nicotine did not affect dSAT performance. We will return to the analysis of this data in conjunction with the effects of co-administration of this dose of nicotine and MLA. We will next describe the electrochemical evidence, as this evidence justifies the co-administration experiment.
Larger and ‘Sharper’ Cholinergic Transients Evoked by S 38232 When Compared with Nicotine
We earlier showed that nAChR agonists evoke transient increases in ACh release in the prefrontal cortex. We also identified major aspects of the underlying neuronal mechanisms. This evidence supports the hypothesis that the greater pro-attentional efficacy of selective α4β2* nAChR agonists is related to their ability to evoke larger and ‘sharper’ cholinergic transients than nicotine (Parikh et al, 2008; Sarter et al, 2009b). Thus, we determined the cholinergic transients evoked by S 38232 and compared their amplitudes and decay rates with those evoked by nicotine (Parikh et al, 2008).
The in vitro electrochemical properties of choline-sensitive electrodes used in these experiments are described in Table 1 in Supplementary data. Administration of S 38232 (40, 200, and 2000 pmol) evoked cholinergic transients that were characterized by dose-dependent increases in amplitude (F(2,13)=29.05; p<0.001; post hoc LSDs indicated that the amplitude after the two higher doses was larger than the amplitude evoked by 40 pmol; Figure 3a and d). Consistent with the classification of S 38232 as a selective α4β2* nAChR agonist, the amplitude of the cholinergic transient evoked by S 38232 (2 nmol) was almost completely attenuated by co-administration of the relatively α4β2*-selective antagonist DHβE (1.6 nmol; residual amplitude: 1.43±0.19 μM; t(5)=5.07; p=0.007).
Transient increases in prefrontal acetylcholine release evoked by S 38232 and nicotine (the data on nicotine are used for comparison and were adopted from Parikh et al, 2008). (a, b) provide examples of individual traces evoked by S 38232 (a) and nicotine (b; arrows indicates the time of drug administration). These traces exemplify the strikingly ‘sharper’ transients evoked by the α4β2* nAChR agonist when compared with the slower decay rate of nicotine-evoked cholinergic transients. The slower decay of nicotine-evoked transients indicates ongoing and only slowly decreasing acetylcholine release; (b) also illustrates the ‘sharpening’ of nicotine-evoked cholinergic transients by blocking the α7 nAChR with MLA. (c) The time required for transients to reach peak amplitude (‘rise time’) increased dose dependently for nicotine, but not for S 38232; indeed, the rise time for transients evoked by 2000 pmol of S 38232 did not differ from rise times of transients evoked by 200 or 40 pmol. Furthermore, by the second highest dose of drug (200 pmol), nicotine-evoked transients required significantly more time to reach peak amplitude when compared with α4β2* nAChR agonist-evoked transients. The two individual data points shown in (c) indicate that blocking the α7 nAChR, by co-administration of MLA, shortened the rise time of nicotine-evoked cholinergic transients. (d) S 38232 was more potent, but not more efficacious, with respect to the peak amplitudes of cholinergic transients. The two lower doses of S 38232 evoked significantly larger amplitudes than similar doses of nicotine. The two individual data points in (d) indicate that blocking the α7 nAChR did not robustly reduce the amplitudes of nicotine-evoked transients. As described in Results, blocking α4β2* nAChR almost completely attenuated the amplitudes that were evoked by S 38232 (2 nmol). (e) Transients evoked by nicotine were relatively slow to return to baseline, requiring 70 s after the highest dose to decrease to 50% of peak current (t50). In contrast, t50 values of transients evoked by S 38232 were largely flat across doses and remained under 10 s.Co-administration of MLA accelerated the decay rate of nicotine-evoked cholinergic signals, reducing t50 values close to those for transients evoked by the selective α4β2* nAChR agonist (see individual data points). Taken together, the results shown in (c–e) indicate that S 38232 evokes ‘sharper’ cholinergic transients than nicotine.
Compared with the amplitudes of cholinergic transients evoked by nicotine (40 and 200 pmol, 4 and 20 nmol; Parikh et al, 2008), S 38232 was significantly more potent than nicotine in evoking cholinergic transients (Figure 3d). Comparisons between the amplitudes evoked by the two lower doses of S 38232 indicated larger cholinergic signal amplitudes compared with the amplitudes evoked by identical doses of nicotine (40 pmol: t(8)=3.94; p=0.004; 200 pmol: t(8)=3.36; p=0.01). The amplitude produced by the highest dose of S 38232 corresponded with that evoked by the highest dose of nicotine (20 nmol; p=0.59). As illustrated in Figure 3d, amplitudes generally reached a plateau at 5.5–6 μM, indicating that the greater potency of the selective agonist was not associated with greater efficacy.
Cholinergic transients evoked by S 38232 were robustly ‘sharper’ than those evoked by nicotine. First, as illustrated in Figure 3c, dose of S 38232 did not affect the relatively short rise time of transients evoked by this compound (time from administration of the compound to peak amplitude; F(2,15)=0.15; p=0.858; Figure 3c; 5.73±0.28 s). In contrast, nicotine-evoked signals required robustly more time to reach peak amplitude, up to almost 30 s for the highest dose (note again that peak amplitudes did not differ between the highest dose of S 38232 and nicotine; above). Even at the second dose, 200 pmol, nicotine-evoked signals were slower to reach peak amplitude (nicotine: 21.75±7.60 s; S 38232: 5.94±1.04 s; t(8)=2.62; p=0.03).
Second, as illustrated in Figure 3e, t50 values of cholinergic signals evoked by S 38232 remained below 10 s even after the highest dose, contrasting with nicotine-evoked signals that required almost 70 s to decline by 50% from peak values after the highest dose. Dose of S 38232 affected the time required for the amplitude of cholinergic transients to decrease by 50% from peak levels (t50) (F(2,15)=4.14; p=0.041). However, post hoc LSDs revealed that this effect was due to a relatively small increase in t50 (about 2 s) after the administration of 200 pmol when compared with the effects of the lower and higher dose (40 pmol and 2 nmol; Figure 3e). Even at the second dose, 200 pmol, nicotine-evoked signals were significantly slower to decay (t50; nicotine: 39.75±12.43 s; S 38232: 9.95±0.72 s; t(8)=2.82; p=0.02). Collectively, these results indicate that S 38232 evokes cholinergic transients with greater potency when compared with nicotine, and that cholinergic signals evoked by S 38232 differ from those resulting from nicotine with regard to rise times and decay rates, yielding robustly ‘sharper’ cholinergic transients evoked by S 38232.
Blockade of α7 nAChR ‘Sharpens’ Nicotine-Evoked Transients
As illustrated in Figure 3b–e, nicotine-evoked cholinergic transients were characterized by slower rise times and decay rates when compared with those evoked by the selective α4β2* nAChR agonist. We earlier observed that blockade of the α7 nAChR with MLA did not affect the amplitude of nicotine-evoked cholinergic transients, but partly attenuated the slow rise time and the slow decay rate of nicotine-evoked transients (Figure 3b–e; these data were taken from Parikh et al, 2008 and integrated into Figure 3 to provide a justification for the test of the effects of the co-administration of nicotine and MLA on dSAT performance). More recently, we determined the effects of nicotine in mice lacking the α7 nAChR and again found that the slow rise time and decay rate of nicotine-evoked cholinergic signals are partly mediated through the α7 nAChR (Parikh et al, 2010). Thus, with respect to cholinergic transients, blocking the α7 nAChR converts nicotine into a more selective α4β2* nAChR agonist.
Co-administration of Nicotine and MLA Enhances dSAT Performance
Compared with the administration of saline or nicotine alone (0.1 mg/kg), co-administration of this dose of nicotine and MLA (1.0 mg/kg) enhanced the relative number of hits during dSAT performance. As indicated in Materials and methods, we also tested a higher dose of MLA (5.0 mg/kg); however, co-administration of nicotine and the higher dose of MLA impaired performance, likely reflecting non-selective antagonist effects of MLA (see Discussion in López-Hernández et al, 2009). Therefore, these data are not described.
Compared with vehicle and nicotine administered alone, the co-administration of nicotine and MLA enhanced the hit rate across all three blocks of trials of dSAT performance (main effect of treatment: F(2,16)=5.46; p=0.016; see Figure 2e). Figure 2d shows effects over blocks to allow comparisons between the effects of S 38232 and the co-administration treatment. Although this figure suggests that the co-treatment increased hits particularly robustly during the post-distractor block, the effects of treatment did not interact with block (p=0.18).
DISCUSSION
The results of the experiments described above indicate that administration of a selective α4β2* nAChR agonist, but not nicotine, facilitates attentional performance under taxing conditions. Compared with nicotine, the selective α4β2* nAChR agonist evoked ‘sharper’ cholinergic transients, which mirrored the transients that mediate cue detection in performing animals. This finding is consistent with the hypothesis that such selective agonists are able to amplify without broadening such transients, and thereby benefit the detection of signals in attention tasks. The more slowly rising and decaying transients evoked by nicotine are ‘sharpened’ by blocking the α7 nAChR; accordingly, we found that co-administration of nicotine with MLA robustly increased the hit rate of dSAT-performing animals. The discussion below will focus on (a) the lack of beneficial effects of nicotine, (b) the cognitive and neuronal mechanisms underlying the attentional effects of the selective α4β2* nAChR agonist, (c) the prediction of attentional enhancement based on the characteristics of nAChR agonist-evoked cholinergic transients, and (d) the implication of these findings for strategies focusing on the treatment of the cognitive impairments associated with a range of disorders.
As noted in the Introduction, the demonstration of beneficial attentional effects of nicotine in healthy, non-smoking human beings and intact animals has been less than straightforward. Here, as well as in earlier studies, we failed to show beneficial effects of nicotine on SAT performance (Turchi et al, 1995). In addition, and in agreement with the results described above, Bushnell et al (1997) reported a decrease in hits after their highest dose of nicotine (0.26 mg/kg; base weight) using a SAT task similar to the one used in this study. As already mentioned, the demonstration of beneficial effects of nicotine on the performance of the five-choice serial reaction time task (5CSRTT) depends on specific parameters, and effects on response accuracy were not consistently reported (references in Introduction). Thus, in the absence of additional demands on attentional control, acute enhancement of attentional performance by nicotine has been difficult to show in intact animals. However, the collective evidence suggests that 5CSRTT performance may be more readily enhanced than SAT performance (references in Introduction; see also Stolerman et al, 2000). The two tasks differ primarily in that the 5CSRTT does not involve non-signal trials, or the randomized presentation of signal and non-signal trials within a test session. Furthermore, SAT-performing animals remain positioned in front of the intelligence panel throughout the session, operating the left and right lever most of the time using left and right forepaws and relatively rarely engage in competitive behaviors. Thus, multiple cognitive and behavioral mechanisms may be speculated to account for the task-based difference in the efficacy of nicotine.
Given that the available evidence suggests that beneficial attentional effects of nicotine can be more readily shown in interaction with increased demands on attentional control (references in Introduction; Hahn et al, 2002), the failure of nicotine to benefit dSAT performance was unexpected. As indicated in Figure 2d, after the administration of nicotine, there was a descriptive trend for an increase in hits in the post-distractor period; however, statistical power estimates indicate that for this effect to reach significance data from over 100 animals would be needed. Were it not for the robust effects of S 38232 and nicotine/MLA co-treatment, we would need to conclude that the dSAT does not adequately tax attentional control. However, given the effects of these two treatments, the limited efficacy of nicotine is more likely related to its non-selective pharmacological and associated electrochemical profile (below).
In contrast to nicotine, the selective α4β2* nAChR agonist robustly enhanced post-distractor dSAT performance. Although the evidence from studies in human beings, including patients, and animal experiments remains limited, such ligands seem to produce more reliable and perhaps more robust enhancement of attentional performance than nicotine (McGaughy et al, 1999; Wilens et al, 1999, 2006; Grottick and Higgins, 2000; Dunbar et al, 2007; Wilens and Decker, 2007).
The detection of signals requires transient increases in cholinergic activity in the prefrontal cortex (Parikh et al, 2007). Ideally, the effects of nicotine and α4β2*-selective nAChR agonists on such transients recorded in performing animals would be expected to reveal the basis for their differential efficacy. Unfortunately, such studies remain technically extremely challenging and, therefore, the present evidence requires extrapolation from the characteristics of nAChR agonist-evoked transients recorded in anesthetized animals to modulation of detection-mediating transients. However, the little data that is available suggests that such an extrapolation may be feasible and informative (Sarter et al, 2009a).
Our collective electrochemical evidence supports a model indicating that during cue detection, cholinergic transients are a product of local prefrontal glutamatergic–cholinergic interactions (Parikh et al, 2008, 2010). The initial ACh release is augmented by cholinergic stimulation of α4β2* nAChRs that are situated on the terminals of thalamic glutamatergic inputs, and the subsequent stimulation of ionotropic glutamate receptors. The parsimonious model posits that glutamate receptors can be located on cholinergic terminals (Sarter et al, 2009a), and predicts, as indicated by the current data (Figure 3), that α4β2* nAChR agonists potently evoke cholinergic transients. Our prior data also suggest that the amplitude of cholinergic transients evoked by nicotine is controlled by the effects of nicotine at α4β2* nAChRs. In contrast, the slow rise time and decay rate of nicotine-evoked cholinergic transients, indicative of slowly increasing, more lasting, and more slowly diminishing ACh release, are due in part to stimulation of α7 nAChRs. The rise time and decay rates of transients evoked by S 38232-evoked transients suggest that the low affinity of this compound for α7 nAChR (see Materials and methods) remains irrelevant in vivo.
The enhancement of attentional performance by S38232 is consistent with the hypothesis that such compounds are able to augment, without widening, cholinergic transients, thereby enhancing the efficacy and rate of successful cue detection. It is less clear whether the lower rise time, the slower decay rate of nicotine-evoked transients, or both limit the efficacy of the non-selective nAChR agonist. If the early increase in cholinergic activity, before initiation of behavior, is what truly fosters cue detection (Parikh et al, 2007), then such slow rise times would not be predicted to benefit detection performance. Alternatively, the slow temporal dynamics of nicotine-evoked increases in cholinergic neurotransmission may be insufficient to effectively enhance discrete behavioral or cognitive operations.
Although the above discussion remains necessarily speculative, the finding that the co-administration of nicotine with MLA ‘sharpens’ nicotine-evoked cholinergic transients and enhances the hit rate in dSAT-performing animals considerably substantiates the suggestion that the cholinergic signature of nAChR agonists predicts attentional performance effects. Inspection of the data indicates that S 38232 and the nicotine/MLA co-treatment resulted in similar hit rates during the recovery period after the distractor block (55–60% hits; Figure 2c and d). Taken together, these findings are consistent with the hypothesis that stimulation of α4β2* nAChRs is sufficient for enhancing attentional performance. These results and associated hypotheses suggest that it is less likely that stimulation of prefrontal α7 nAChRs benefits the detection of cues in attentional contexts (eg Grottick and Higgins, 2000; Grottick et al, 2003; Hahn et al, 2003; Paolone et al, 2009).
The present evidence indicates the usefulness of the behavioral and electrochemical research approaches for finding and developing compounds designed to enhance attentional performance. First, the dSAT seems sufficiently taxing to reveal the beneficial effects of selective nAChR agonists. The focus on dSAT performance over performance of the SAT is of clinical relevance, as in many groups of patients with neuropsychiatric and neurodegenerative disorders or brain injury, attentional impairments are a function of the demands on effort and top-down control (eg Stulemeijer et al, 2007; Nuechterlein et al, 2009; Sarter et al, 2009b). Such demands further activate prefrontal circuitry, in part because of greater demands on cholinergic activity (Kozak et al, 2006). Second, the current evidence indicates that the characterization of the features of cholinergic transients, evoked by local administration and in anesthetized animals, may serve as an informative neuropharmacological screening procedure for putative cognition enhancers. Although it will be necessary to further show that the effects on amplitudes and decay rates of such transients in anesthetized animals predict the modulation of such transients in performing animals, the present results substantiate the hypothesis that compounds, which are able to evoke ‘sharp,’ transient increases in ACh release enhance attentional performance.
References
Bizarro L, Stolerman IP (2003). Attentional effects of nicotine and amphetamine in rats at different levels of motivation. Psychopharmacology (Berl) 170: 271–277.
Blondel A, Sanger DJ, Moser PC (2000). Characterization of the effects of nicotine in the five-choice serial reaction time task in rats: antagonist studies. Psychopharmacology (Berl) 149: 293–305.
Bushnell PJ, Oshiro WM, Padnos BK (1997). Detection of visual signals by rats: effects of chlordiazepoxide and cholinergic and adrenergic drugs on sustained attention. Psychopharmacology (Berl) 134: 230–241.
Demeter E, Sarter M, Lustig C (2008). Rats and humans paying attention: cross-species task development for translational research. Neuropsychology 22: 787–799.
Dunbar GC, Inglis F, Kuchibhatla R, Sharma T, Tomlinson M, Wamsley J (2007). Effect of ispronicline, a neuronal nicotinic acetylcholine receptor partial agonist, in subjects with age associated memory impairment (AAMI). J Psychopharmacol 21: 171–178.
Greenwald AG, Gonzalez R, Harris RJ, Guthrie D (1996). Effect sizes and p values: what should be reported and what should be replicated? Psychophysiology 33: 175–183.
Grottick AJ, Haman M, Wyler R, Higgins GA (2003). Reversal of a vigilance decrement in the aged rat by subtype-selective nicotinic ligands. Neuropsychopharmacology 28: 880–887.
Grottick AJ, Higgins GA (2000). Effect of subtype selective nicotinic compounds on attention as assessed by the five-choice serial reaction time task. Behav Brain Res 117: 197–208.
Hagan JJ, Jones DN (2005). Predicting drug efficacy for cognitive deficits in schizophrenia. Schizophr Bull 31: 830–853.
Hahn B, Sharples CG, Wonnacott S, Shoaib M, Stolerman IP (2003). Attentional effects of nicotinic agonists in rats. Neuropharmacology 44: 1054–1067.
Hahn B, Shoaib M, Stolerman IP (2002). Nicotine-induced enhancement of attention in the five-choice serial reaction time task: the influence of task demands. Psychopharmacology (Berl) 162: 129–137.
Johnston K, Levin HM, Koval MJ, Everling S (2007). Top-down control-signal dynamics in anterior cingulate and prefrontal cortex neurons following task switching. Neuron 53: 453–462.
Kozak R, Bruno JP, Sarter M (2006). Augmented prefrontal acetylcholine release during challenged attentional performance. Cereb Cortex 16: 9–17.
Kozak R, Martinez V, Young D, Brown H, Bruno JP, Sarter M (2007). Toward a neuro-cognitive animal model of the cognitive symptoms of schizophrenia: disruption of cortical cholinergic neurotransmission following repeated amphetamine exposure in attentional task-performing, but not non-performing, rats. Neuropsychopharmacology 32: 2074–2086.
Lagostena L, Danober L, Challal S, Lestage P, Mocaer E, Trocme-Thibierge C et al (2010). Modulatory effects of S 38232, a non α7 containing nicotine acetylcholine receptor agonist on network activity in the mouse hippocampus. Neuropharmacology (e-pub ahead of print).
Levin ED, Connors CK, Silva D, Hinton SC, Meck WH, March J et al (1998). Transdermal nicotine effects on attention. Psychopharmacology (Berl) 140: 135–141.
Lippiello P, Letchworth SR, Gatto GJ, Traina VM, Bencherif M (2006). Ispronicline: a novel alpha4beta2 nicotinic acetylcholine receptor-selective agonist with cognition-enhancing and neuroprotective properties. J Mol Neurosci 30: 19–20.
López-Hernández GY, Thinschmidt JS, Zheng G, Zhang Z, Crooks PA, Dwoskin LP et al (2009). Selective inhibition of acetylcholine-evoked responses of alpha7 neuronal nicotinic acetylcholine receptors by novel tris- and tetrakis-azaaromatic quaternary ammonium antagonists. Mol Pharmacol 76: 652–666.
Manusco G, Warburton DM, Melen M, Sherwood N, Tirelli E (1999). Selective effects of nicotine on attentional processes. Psychopharmacology (Berl) 146: 199–204.
McGaughy J, Decker MW, Sarter M (1999). Enhancement of sustained attention performance by the nicotinic acetylcholine receptor agonist ABT-418 in intact but not basal forebrain-lesioned rats. Psychopharmacology (Berl) 144: 175–182.
McGaughy J, Kaiser T, Sarter M (1996). Behavioral vigilance following infusions of 192 IgG-saporin into the basal forebrain: selectivity of the behavioral impairment and relation to cortical AChE-positive fiber density. Behav Neurosci 110: 247–265.
Mirza NR, Bright JL (2001). Nicotine-induced enhancements in the five-choice serial reaction time task in rats are strain-dependent. Psychopharmacology (Berl) 154: 8–12.
Mirza NR, Stolerman IP (1998). Nicotine enhances sustained attention in the rat under specific task conditions. Psychopharmacology (Berl) 138: 266–274.
Newhouse PA, Potter A, Singh A (2004). Effects of nicotinic stimulation on cognitive performance. Curr Opin Pharmacol 4: 36–46.
Nuechterlein KH, Luck SJ, Lustig C, Sarter M (2009). CNTRICS final task selection: control of attention. Schizophr Bull 35: 182–196.
Paolone G, Ji J, Williams S, Howe WM, Ward J, Parikh V et al (2009). Effects of the selective alpha 7 nAChR agonist ABT-107 on prefrontal glutamatergic and cholinergic activity and attentional performance. Society for Neuroscience Annual Meeting (poster no. 227.5), Chicago, IL.
Parikh V, Kozak R, Martinez V, Sarter M (2007). Prefrontal acetylcholine release controls cue detection on multiple timescales. Neuron 56: 141–154.
Parikh V, Man K, Decker MW, Sarter M (2008). Glutamatergic contributions to nicotinic acetylcholine receptor agonist-evoked cholinergic transients in the prefrontal cortex. J Neurosci 28: 3769–3780.
Parikh V, Jinzhao J, Decker MW, Sarter M (2010). Prefrontal β2 subunit-containing and α7 nAChRs differentially control prefrontal glutamatergic and cholinergic signaling. J Neurosci (in press).
Potter A, Corwin J, Lang J, Piasecki M, Lenox R, Newhouse PA (1999). Acute effects of the selective cholinergic channel activator (nicotinic agonist) ABT-418 in Alzheimer's disease. Psychopharmacology (Berl) 142: 334–342.
Prendergast MA, Jackson WJ, Terry AVJ, Decker MW, Arneric SP, Buccafusco JJ (1998). Central nicotinic receptor agonists ABT-418, ABT-089, and (-)-nicotine reduce distractibility in adult monkeys. Psychopharmacology (Berl) 136: 50–58.
Rusted JM, Caulfield D, King L, Goode A (2000). Moving out of the laboratory: does nicotine improve everyday attention? Behav Pharmacol 11: 621–629.
Sahakian B, Jones G, Levy R, Gray J, Warburton D (1989). The effects of nicotine on attention, information processing, and short-term memory in patients with dementia of the Alzheimer type. Br J Psychiatry 154: 797–800.
Sarter M (2006). Preclinical research into cognition enhancers. Trends Pharmacol Sci 27: 602–608.
Sarter M (2010). Attention. In: Stolerman IP (ed). Encyclopedia of Psychopharmacology. Springer (in press): Berlin. In press.
Sarter M, Gehring WJ, Kozak R (2006). More attention must be paid: the neurobiology of attentional effort. Brain Res Rev 51: 145–160.
Sarter M, Hasselmo ME, Bruno JP, Givens B (2005). Unraveling the attentional functions of cortical cholinergic inputs: interactions between signal-driven and cognitive modulation of signal detection. Brain Res Rev 48: 98–111.
Sarter M, Martinez V, Kozak R (2009b). A neurocognitive animal model dissociating between acute illness and remission periods of schizophrenia. Psychopharmacology (Berl) 202: 237–258.
Sarter M, Parikh V, Howe WM (2009a). nAChR agonist-induced cognition enhancement: integration of cognitive and neuronal mechanisms. Biochem Pharmacol 10: 658–667.
Stolerman IP, Mirza NR, Hahn B, Shoaib M (2000). Nicotine in an animal model of attention. Eur J Pharmacol 393: 147–154.
Stulemeijer M, Andriessen TM, Brauer JM, Vos PE, Van Der Werf S (2007). Cognitive performance after mild traumatic brain injury: the impact of poor effort on test results and its relation to distress, personality and litigation. Brain Inj 21: 309–318.
Turchi J, Holley LA, Sarter M (1995). Effects of nicotinic acetylcholine receptor ligands on behavioral vigilance in rats. Psychopharmacology (Berl) 118: 195–205.
Weissman DH, Warner LM, Woldorff MG (2004). The neural mechanisms for minimizing cross-modal distraction. J Neurosci 24: 10941–10949.
Wilens TE, Biederman J, Spencer TJ, Bostic J, Prince J, Monuteaux MC et al (1999). A pilot controlled clinical trial of ABT-418, a cholinergic agonist, in the treatment of adults with attention deficit hyperactivity disorder. Am J Psychiatry 156: 1931–1937.
Wilens TE, Decker MW (2007). Neuronal nicotinic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: focus on cognition. Biochem Pharmacol 74: 1212–1223.
Wilens TE, Verlinden MH, Adler LA, Wozniak PJ, West SA (2006). ABT-089, a neuronal nicotinic receptor partial agonist, for the treatment of attention-deficit/hyperactivity disorder in adults: results of a pilot study. Biol Psychiatry 59: 1065–1070.
Acknowledgements
This research was support in part by PHS grants MH080426 and MH080332 and by a grant from Institut de Recherches Internationales Servier (Courbevoie, France). WMH was also supported by the PHS Training Grant T32 DA007267.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
This research was support in part by PHS grants MH080426 and MH080332 and by a grant from Institut de Recherches Internationales Servier (Courbevoie, France). WMH. was also supported by the PHS Training Grant T32 DA007267 (University of Michigan Substance Abuse Research Center; UMSARC). Listing for each author, detailing the names of organizations, institutions, companies, and individuals, including intermediaries such as sub-contractors or conference organizers, from whom they have received compensation for professional services in any of the earlier 3 years, or from whom they anticipate receiving such compensation in the near future, whether or not these affiliations appear to have any relevance to the topic covered in the submission are as follows: William M Howe, Jinzaho Ji, Vinay Parikh, Sarah Williams declare no conflict of interest Dr Sarter has received honoraria for speaking at Abbott Laboratories and Pfizer Pharmaceuticals and has received research support from Abbott Laboratories, Pfizer Pharmaceuticals, and Institut de Recherches Internationales Servier. Elisabeth Mocaër and Caryn Trocmé-Thibierge are employed by the Institut de Recherches Internationales Servier.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Howe, W., Ji, J., Parikh, V. et al. Enhancement of Attentional Performance by Selective Stimulation of α4β2* nAChRs: Underlying Cholinergic Mechanisms. Neuropsychopharmacol 35, 1391–1401 (2010). https://doi.org/10.1038/npp.2010.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2010.9
Keywords
This article is cited by
-
Xanomeline restores endogenous nicotinic acetylcholine receptor signaling in mouse prefrontal cortex
Neuropsychopharmacology (2023)
-
Chemogenetic inhibition of prefrontal projection neurons constrains top–down control of attention in young but not aged rats
Brain Structure and Function (2021)
-
Dissociation of nicotinic α7 and α4/β2 sub-receptor agonists for enhancing learning and attentional filtering in nonhuman primates
Psychopharmacology (2020)
-
Evidence for positive allosteric modulation of cognitive-enhancing effects of nicotine in healthy human subjects
Psychopharmacology (2020)
-
Behavioural and pharmacological profiles of zebrafish administrated pyrrolidinyl benzodioxanes and prolinol aryl ethers with high affinity for heteromeric nicotinic acetylcholine receptors
Psychopharmacology (2020)