Abstract
Patients with prolonged seizures that do not respond to intravenous benzodiazepines and a second-line anticonvulsant suffer from refractory status epilepticus and those with seizures that do not respond to continuous intravenous anesthetic anticonvulsants suffer from super-refractory status epilepticus. Both conditions are associated with significant morbidity and mortality. A strict pharmacological treatment regimen is urgently required, but the level of evidence for the available drugs is very low. Refractory complex focal status epilepticus generally does not require anesthetics, but all intravenous non-anesthetizing anticonvulsants may be used. Most descriptive data are available for levetiracetam, phenytoin and valproate. Refractory generalized convulsive status epilepticus is a life-threatening emergency, and long-term clinical consequences are eminent. Administration of intravenous anesthetics is mandatory, and drugs acting at the inhibitory gamma-aminobutyric acid (GABA)A receptor such as midazolam, propofol and thiopental/pentobarbital are recommended without preference for one of those. One in five patients with anesthetic treatment does not respond and has super-refractory status epilepticus. With sustained seizure activity, excitatory N-methyl-d-aspartate (NMDA) receptors are increasingly expressed post-synaptically. Ketamine is an antagonist at this receptor and may prove efficient in some patients at later stages. Neurosteroids such as allopregnanolone increase sensitivity at GABAA receptors; a Phase 1/2 trial demonstrated safety and tolerability, but randomized controlled data failed to demonstrate efficacy. Adjunct ketogenic diet may contribute to termination of difficult-to-treat status epilepticus. Randomized controlled trials are needed to increase evidence for treatment of refractory and super-refractory status epilepticus, but there are multiple obstacles for realization. Hitherto, prospective multicenter registries for pharmacological treatment may help to improve our knowledge.
Similar content being viewed by others
After failure of two intravenous anticonvulsant drugs, ongoing epileptic seizures require consequent, pharmacological treatment that depends on the severity of seizures. |
Refractory complex focal status epilepticus should be treated with compounds that do not cause significant sedation and that do not require mechanical ventilation. |
Refractory generalized convulsive status epilepticus should be treated with strong-acting anesthetic drugs to suppress seizure activity as soon as possible. |
Continuing seizures or recurring seizures after anesthetics are challenging and drugs with a wide range of mechanisms of action may be administered. |
1 Introduction
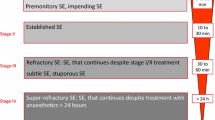
From an epileptologist point of view, status epilepticus is a rare condition as almost all epileptic seizures are self-limiting events. From the emergency physician’s point of view, status epilepticus is frequent, and is the second most common neurological emergency after stroke. Most epidemiological studies report incidence rates for status epilepticus of 10–20 per 100,000, although a higher incidence was found in one US study (41–61 per 100,000) [1]. In about one-third of cases, status epilepticus is refractory towards first-line intravenous benzodiazepines and second-line non-anesthetic anticonvulsants [2,3,4]. In 20% of patients requiring treatment with anesthetic anticonvulsants for refractory status epilepticus, seizure activity even continues after administration of these anesthetics, a condition termed malignant or super-refractory status epilepticus [5, 6]. The incidence rate for super-refractory status epilepticus has been reported to be 0.7/100,000 in Finland and 3.0/100,000 in Germany [7, 8].
Refractory and super-refractory status epilepticus are associated with significant morbidity and mortality [9]. In one study, 1-year mortality was 22% for refractory and 36% for super-refractory status epilepticus [8], in another study, accordant discharge mortality was 15 and 40% [7]. Status epilepticus is a relevant burden to health-care systems. Direct cost of illness for all types of status epilepticus were US$8400 (median, admittance to US hospitals in the years 1993 and 1994), costs doubled to US$16,900 when etiology was an acute central nervous system disorder which commonly results in refractory status epilepticus [10]. More recent data from Germany covering the years 2008–2013 indicate median direct costs for each case with refractory and super-refractory status epilepticus of €4600 and €32,700, respectively [7]. Very similar novel data (year 2012) are available from US hospitals with median direct cost for hospitalization for super-refractory status epilepticus of US$33,300 [11]. One has to keep in mind that higher mortality rates and higher costs for refractory and super-refractory status epilepticus have to be attributed also to the underlying etiology.
Nonetheless, optimal treatment for refractory and super-refractory status epilepticus is of utmost importance, and the mainstay is pharmacotherapy. In the last years, a number of comprehensive review articles on the management of status epilepticus have been published [12,13,14,15], one of those on pharmacotherapy appeared in Drugs 2 years ago [16]. This current review article discusses in-depth pharmacological treatment options for refractory and super-refractory status epilepticus, and first- and second-line treatments as well as non-pharmacological approaches are summarized. This review focuses on treatment of adult patients; pharmacotherapy for childhood status epilepticus is covered elsewhere [17, 18]. Anoxic–hypoxic encephalopathy is excluded from this review, as there is no general agreement on the epileptic nature of clinical and electroencephalographic abnormalities seen in this condition.
2 Definitions
In the year 2015, the Commission on Classification and Terminology and the Commission on Epidemiology of the International League Against Epilepsy have proposed a new definition of status epilepticus [19]. The definition conceptualizes two operational dimensions. Time point “T1” defines the duration of sustained seizure activity after which an epileptic seizure is status epilepticus and after which acute anticonvulsant treatment should be initiated. Time point “T2” defines the duration of sustained seizure activity after which patients are at risk of long-term consequences and after which seizure activity ideally should have been terminated. T1 and T2 differ in regard to type of status epilepticus, that is 5 and 30 min in generalized convulsive status epilepticus, 10 and > 60 min in complex focal status epilepticus and 10–15 min and unknown in absence status epilepticus.
There is no “official” definition of refractory status epilepticus of the International League Against Epilepsy, but most authors agree on refractoriness after failure of a first-line intravenous or intramuscular long-acting benzodiazepine and of a second-line intravenous non-anesthetizing anticonvulsant [15].
Status epilepticus that continues with or rapidly recurs after treatment with continuous intravenous anesthetic anticonvulsants has initially been termed “malignant” [5], and later on the term “super-refractory” was introduced [20] and has become widely accepted.
3 Consequences of Ongoing Seizure Activity
Acute, potentially life-threatening complications and long-term neurocognitive and neurological consequences are the main determinants for the extent of aggressiveness of pharmacological treatment of refractory and super-refractory status epilepticus. The risks of prolonged status epilepticus need to be weighed against the risks of aggressive treatment approaches.
Generalized convulsive status epilepticus results in significant release of endogenous catecholamines. Consequences are arterial hypertension, potentially lethal tachyarrhythmias, pulmonary edema requiring mechanical ventilation, renal failure, disseminated intravascular coagulation, etc. [21]. In generalized convulsive status epilepticus, the mortality risk is 3% within the first 30 min and 19% after more than 30 min [22]. Even if generalized convulsive status epilepticus becomes subtle after some hours, excitotoxicity of persistent generalized epileptiform discharges still has the potential for deleterious effects on the brain [23]. Therefore, generalized convulsive status epilepticus, either overt or subtle, requires prompt treatment escalation if the condition becomes refractory or super-refractory.
Complex focal status epilepticus does not produce acute systemic complications, but patients may be at risk for injuries due to impaired consciousness. Neuronal and clinical long-term consequences, however, are methodologically difficult to assess. If patients have an acute brain disorder, such as encephalitis, as underlying cause of complex focal status epilepticus, consequences of ongoing seizure activity are difficult to discern from those of encephalitis [24]. Though some surrogate markers, such as cortical atrophy demonstrated by neuroimaging [25] or elevated levels neuron-specific enolase in cerebrospinal fluid or serum [26, 27], indicate neuronal damage in refractory complex focal status epilepticus, so far convincing data on clinical long-term consequences of refractory complex focal status epilepticus itself are lacking.
4 Pharmacological Management
4.1 Anticonvulsant Compounds Used in Status Epilepticus
In the following, we discuss individual anticonvulsants with regard to their mechanisms of action, to findings from experimental animal models and to general safety issues with rapid intravenous loading. Compounds are presented in alphabetical order. Data on efficacy are presented in the subchapters on different clinical forms and stages of status epilepticus.
4.1.1 Benzodiazepines
The predominant pharmacological action of benzodiazepines is mediated through high affinity to the allosteric modulatory site on gamma-aminobutyric acid (GABA)A receptors [28]. Benzodiazepines enhance affinity and binding of GABA to the GABAA receptor, thereby increasing the frequency of chloride channel openings [29, 30]. Intracellular influx of chloride ions result in neuronal hyperpolarization [31].
In an animal model of self-sustaining status epilepticus (SSSE) induced in rats by intermittent stimulation of the perforant path, diazepam administered prior to stimulation prevented status epilepticus in all animals [32]. This benzodiazepine was less effective when administered after 30 min of stimulation, efficacy further decreased with longer duration of stimulation. Lorazepam was assessed in an experimental model system of secondary generalized convulsive status epilepticus, brain concentrations peaked 10 min after peak serum levels were achieved [33]. The data suggested that a serum concentration of 0.2 mg/L should be effective in most cases and should provide seizure protection for 24 h following treatment. Diazepam is more lipophilic than lorazepam, which results in rapid redistribution to lipid tissue beyond the brain [34]. This may explain diazepam’s disadvantageous shorter duration of action in the brain compared to lorazepam [35].
4.1.2 Brivaracetam
Brivaracetam is an analogue of levetiracetam, which binds to the synaptic vesicle protein 2A and decreases release of excitatory neurotransmitters [36]. Brivaracetam differs significantly from levetiracetam by its selective, high affinity and differential interaction with synaptic vesicle protein 2A. In preclinical seizure and epilepsy studies, these characteristics correlated with stronger anticonvulsant effects and more rapid onset of action [37].
In the classical rat model of SSSE induced by perforant path stimulation, treatment with brivaracetam resulted in dose-dependent reduction in duration of status epilepticus and cumulative seizure time [38]. Co-administration of low-dose diazepam allowed to reduce the dose of brivaracetam by factor 30 to achieve similar anticonvulsant effects.
Tolerability of intravenous brivaracetam has been demonstrated in a multicenter, randomized controlled trial on 105 patients with focal or generalized epilepsy [39].
4.1.3 Inhalational Anesthetics
Mechanisms of actions of inhalational anesthetics comprise altered activity of neuronal ion channels, particularly at fast synaptic neurotransmitter receptors such as nicotinic acetylcholine, GABAA, and glutamate receptors [40]. This group of anesthetics may also affect neuronal ion channels by binding directly to protein sites. In extracellular voltage recordings from ventral horn interneurons in cultured spinal cord tissue slices obtained from embryonic rats, isoflurane and enflurane significantly reduced spontaneous action potential, the effects were largely mediated by glycine and GABAA receptors [41].
In a model system of penicillin-induced status epilepticus in cats, halothane, isoflurane, and sevoflurane were assessed in regard to their anticonvulsant properties [42]. All volatile anesthetics showed anticonvulsant effects, but isoflurane was the most potent.
4.1.4 Ketamine
Animal models of sustained status epilepticus have demonstrated that with ongoing seizure activity post-synaptic inhibitory GABAA receptors decline in number, and on the other hand, that functionally active excitatory N-methyl-d-aspartate (NMDA) receptors are increasingly expressed (Fig. 1) [43, 44]. Both mechanisms result in increased neuronal excitability. Interestingly, the increase in number of NMDA receptors paves the way to an alternative treatment approach, the pharmacological blockade of the NMDA receptor.
Model of Chen’s and Wasterlain’s hypothesis of receptor trafficking in transition of single seizures to status epilepticus [44]. Top: after repeated seizures, the synaptic membrane of GABAA receptors forms clathrin-coated pits, which internalize as clathrin-coated vesicles (C), inactivating the receptors because they are no longer within reach of the neurotransmitter. These vesicles develop into endosomes (E), which can deliver the receptors to lysosomes (L) where they are destroyed, or to the Golgi apparatus (G) from where they are recycled to the membrane. Bottom: by contrast, in NMDA synapses, subunits are mobilized to the synaptic membrane and assemble into additional receptors. As a result of this trafficking, the number of functional NMDA receptors per synapse increases whereas the number of functional GABAA receptors decreases [43]
Ketamine blocks the ionotropic NMDA receptor, which can produce channels permeable to calcium and sodium ions [45], which themselves mediate fast excitatory neurotransmission in the brain [46]. By this mechanism, ketamine reduces neuronal excitability.
In an animal model of electrically induced status epilepticus, ketamine did not affect seizure activity within the first 15 min after onset but effectively controlled status epilepticus after 60 min when GABAergic phenobarbital had already lost its anticonvulsant potency [47]. These findings nicely demonstrate the progressive pharmacoresistance towards anticonvulsants acting at the GABA receptor and the increasing efficacy of drugs blocking the NMDA receptor. Further experimental data revealed that ketamine and benzodiazepines (diazepam, midazolam) have a strong synergistic effect in status epilepticus [48, 49].
4.1.5 Lacosamide
Lacosamide differs from other sodium channel blockers by its selective effects on slow channel inactivation; it shifts the slow inactivation curve to more hyperpolarized potentials and enhances the maximal fraction of channels that are in the slow inactivated state [50]. Recent data have demonstrated that the efficacy of lacosamide, in regard to inhibition of high-frequency firing, is unabated in both chronic experimental and human epilepsy [51].
In the experimental model of SSSE, rats were treated with lacosamide either 10 or 40 min after onset of perforant path stimulation. Early treatment with lacosamide significantly reduced status epilepticus activity in a dose-dependent manner, while late treatment only showed a trend toward reduced seizure activity [52].
Tolerability of intravenous lacosamide was excellent in lacosamide-naive adult patients with focal epilepsy when administered over 15 min at doses of 200 mg (25 patients) and 300 mg (50 patients), the 400 mg loading dose (25 patients) was less well tolerated [53]. Another study reported 17 adult in-patients who received lacosamide infusion during video-EEG-monitoring (200 mg every 12 h for 2–3 days), rapid loading was well tolerated with few mild or moderate adverse events in 3 out of 17 patients only (17.6%) [54].
4.1.6 Levetiracetam
Unlike other anticonvulsants at the time-point of levetiracetam development, the mechanisms of action involve neuronal binding to synaptic vesicle protein 2A, which inhibits calcium release from intraneuronal stores and thus excessive synchronized neuronal activity [55]. Due to its unique main mechanism of action at that time, this drug threatened to fall through the cracks as it failed to prove efficacy in the classical experimental screening models for compounds with anticonvulsant properties. The maximal electroshock model generally identifies sodium channel blockers [56] and the chemoconvulsant pentylenetetrazole model generally identifies GABAergic drugs [57]. In contrast, levetiracetam demonstrated efficacy in the 6 Hz psychomotor seizure model, which had been developed in the early 1950s [58] but had been mostly ignored since then as it failed to prove efficacy of phenytoin [59].
In the experimental model of SSSE, pretreatment with intravenous levetiracetam reduced or prevented the development of status epilepticus in a dose-dependent manner [60]. Administration of levetiracetam during the maintenance phase of status epilepticus successfully terminated seizure activity. Co-administration of levetiracetam to diazepam exhibited an additive effect.
Tolerability of intravenous levetiracetam has been assessed in 11 adult patients with status epilepticus who had already been treated with benzodiazepines followed by phenytoin or valproic acid [61]. Levetiracetam at 2500 mg was administered over approximately 5 min. No serious adverse events were reported.
4.1.7 Phenobarbital
Barbiturates activate postsynaptic GABAA receptors [62], which results in an opening of the receptor channels leading to chloride ion influx and efflux of bicarbonate ions. Both changes eventually hyperpolarize the cell membrane rendering the neuronal cell less excitable [63, 64]. Barbiturates specifically act via prolonging the opening of the chloride channel [65, 66].
At the beginning of the twentieth century, phenobarbital was approved and marketed as a sedative. The German neurologist Alfred Hauptmann observed that epilepsy patients who were administered this tranquilizer had fewer epileptic seizures [67, 68]. He started to assess the efficacy of phenobarbital systematically and published his observations in 1912 [69]. In 1919, he recommended to extend the use of phenobarbital for the treatment of status epilepticus [70].
In a rat model of generalized convulsive status epilepticus, phenobarbital proved to be efficacious to terminate seizure activity at serum concentrations above 20 mg/L [71].
4.1.8 Phenytoin
Phenytoin is a classical sodium channel blocker which acts via inhibition of sustained repetitive spike firing which may contribute to propagation of epileptic activity [72]. This anticonvulsant binds at the inner pore of the sodium channel in its inactivated state and delays the transition from the inactivated state to the resting closed state that opens with depolarization [73]. Interestingly, the inhibitory properties of the above-mentioned substances are “use-dependent”, i.e. repetitive firing results in greater binding of the drugs and thus enhanced inhibition. This property allows protection against epileptic seizures without major interference with physiological brain function [74].
In the animal model of SSSE induced in rats by brief intermittent perforant path stimulation, intravenous phenytoin at 50 mg/kg was effective in aborting seizure activity when injected 10 min after 30 min stimulation, but efficacy vastly decreased with later injection or longer stimulation [32].
In patients participating in the randomized controlled Veterans Affairs Study, rapid intravenous loading of 18 mg/kg intravenous phenytoin at a rate of 50 mg/min was part of the protocol [2]. One-hundred and one patients were treated with monotherapy phenytoin and 95 with phenytoin co-administered to diazepam; hypoventilation was reported in 9.9%/16.8%, arterial hypotension in 27.0%/31.6% and cardiac arrhythmias in 6.9%/2.1%. These figures were not significantly different compared to patients treated with lorazepam and phenobarbital monotherapy.
4.1.9 Propofol
The mechanism of action of propofol is different from that of barbiturates and benzodiazepines as this compound induces an inward hyperpolarizing current carried by chloride ions [75]. Beyond this direct effect on chloride channel conductance [76], propofol enhances the frequency of GABA-induced conductance events [77] and thus potentiates the inhibitory effect of GABA on neurons [78].
In the SSSE model following 2 h of perforant path stimulation, propofol—even in subanesthetic doses—administered shortly after the end of stimulation and also after 3 h of ongoing status epilepticus terminated seizure activity without recurrence [79].
4.1.10 Thiopental/Pentobarbital
The mechanism of action of thiopental/pentobarbital on the GABAA receptor is somewhat different from benzodiazepines and propofol, as this compound group prolongs the opening of the chloride channel [65, 66, 80].
Thiopental is the barbiturate of choice for treatment of refractory generalized convulsive status epilepticus in Europe, while pentobarbital (the first metabolite of thiopental) is marketed in the USA [81].
4.1.11 Valproic Acid
The exact mechanism by which valproic acid unfolds its anticonvulsant effects is not entirely understood. On the one hand, valproic acid inhibits sustained high-frequency repetitive firing of sodium-dependent action potentials in a use- and voltage-dependent manner [31]. On the other hand, valproic acid may have a GABAergic effect as it increases the concentration of GABA in the whole brain [82, 83] and also increases GABA turnover [84].
In a chemoconvulsant rodent model of generalized convulsive status epilepticus induced by homocysteine thiolactone, valproic acid was able to control seizures at serum concentrations of 270 mg/L [85], the concentrations generally recommended in humans are between 40 and 100 mg/L.
Intravenous infusion of valproic acid in higher doses has been shown to be well tolerated in humans [86].
4.2 Treatment Concepts in Status Epilepticus
With regard to pharmacological treatment, the highest level of evidence is available for first-line drugs in generalized convulsive status epilepticus. In the last 20 years, four randomized controlled trials with sufficient statistical power have been conducted. Though initial treatment of status epilepticus is not the primary focus of this article, the main findings of these trials are summarized; these findings are the basis for subsequent treatment approaches when status epilepticus evolves to be refractory or even super-refractory.
The first multicenter trial (often called Veterans Affairs Study, as patients were recruited in hospitals of the Department of Veterans Affairs in the USA) assessed the efficacy and safety of four different treatment regimens in patients with generalized convulsive status epilepticus. The drugs were administered after patients had arrived in the emergency room [2]. In a total of 384 included patients, intravenous administration of 0.1 mg/kg lorazepam terminated status epilepticus in 64.9% of cases, 15 mg/kg phenobarbital in 58.2%, and 0.15 mg/kg diazepam directly followed by 18 mg/kg phenytoin in 55.8%, there were no significant differences between these groups. In the fourth treatment group, 18 mg/kg phenytoin was administered, which in pairwise comparison to lorazepam was significantly less efficacious (only 43.6% of status epilepticus cases were successfully terminated). Interestingly, the rate of relevant adverse events—hypoventilation, arterial hypotension, and particularly cardiac arrhythmias—did not differ between the treatment groups. Cardiac arrhythmias were observed in 2 and 7% of the regimen incorporating phenytoin, and in 3% and 7% in the two groups without this drug.
Three other high-quality randomized controlled trials have been conducted in the pre-hospital setting. One of those with 205 participants from the San Francisco Bay Area (USA) demonstrated that 2 mg intravenous lorazepam terminate generalized convulsive status epilepticus in 59.1% of cases, while intravenous diazepam at 5 mg was successful in 42.6% of patients [87]. In the placebo group, 21.1% of cases were terminated, which was significantly lower compared to the two benzodiazepine groups and which likely was not a typical placebo effect but spontaneous cessation of seizure activity. It is interesting to note that the dose of lorazepam almost quadruples when treatment is started only in the emergency room [2] compared to earlier out-of-hospital treatment [87]. These clinical data indicate progressive pharmacoresistance to benzodiazepines, which has been explained by erosion of GABAergic inhibition likely due to loss of functionally active post-synaptic GABAA receptors with ongoing seizure activity (Fig. 1) [43, 44]. The second pre-hospital randomized controlled trial (multicenter, USA) aimed to demonstrate non-inferiority of 10 mg intramuscular midazolam (n = 448 patients with generalized convulsive status epilepticus) compared to 4 mg intravenous lorazepam (n = 445 patients), data were collected from patients without established intravenous access at the time point of randomization [88]. Interestingly, intramuscular midazolam (73.4% seizure termination) eventually was superior to intravenous lorazepam (63.4%) in the intention-to-treat analysis. In part, this may be explained by the fact that intramuscular administration is much faster as patients do not need an intravenous line.
In the third pre-hospital randomized controlled trial (multicenter, France), patients with generalized convulsive status epilepticus were randomized to intravenous levetiracetam at 2500 mg co-administered to 1 mg clonazepam (n = 68 patients, seizure termination 74%) and placebo co-administered to 1 mg clonazepam (n = 68 patients, 84%), differences in efficacy were not significant between groups [89].
Another randomized controlled trial from the early 1980 s compared intravenous diazepam (termination rate, 76%) to lorazepam (89%), but this study was slightly underpowered (78 patients with 81 episodes of different clinical forms of status epilepticus, 50% other than generalized convulsive) [90].
Currently, no strong data on second-line anticonvulsants after failure of first-line drugs are available. In the above-mentioned Veterans Affairs Study, each arm contained a second blinded treatment if initial anticonvulsants had failed [2]. Both initial lorazepam and phenobarbital were followed by intravenous phenytoin, while both phenytoin in monotherapy and phenytoin plus diazepam were followed by lorazepam. The four treatment combinations did not differ in regard to efficacy.
Two randomized controlled—but unfortunately underpowered—studies compared each two second-line intravenous anticonvulsants after failure of benzodiazepines. Valproic acid (88% seizure termination) was as efficacious as phenytoin (84%) [91] and as diazepam (56 vs 50%) [92]. A recent meta-analysis on randomized controlled trials assessing efficacy of the intravenous second-line agents levetiracetam versus phenytoin or levetiracetam versus valproic acid for generalized convulsive status epilepticus did not detect any differences, but all studies reviewed were underpowered limiting the significance of the findings [93].
Another meta-analysis incorporating 27 pro- and retrospective studies with 798 patients assessed efficacy to terminate benzodiazepine-resistant generalized convulsive status epilepticus of levetiracetam (68.5% success rate), phenobarbital (73.6%), phenytoin (50.2%), and valproic acid (75.7%) [94], there were no significant differences between these compounds.
So far, no randomized controlled trials on intravenous lacosamide in benzodiazepine-refractory status epilepticus have been conducted. A recent systematic review on the current evidence for lacosamide in status epilepticus mostly relied on retrospective data, overall efficacy was 57% with no relevant differences between non-convulsive and convulsive status epilepticus [95]. There was a significant decrease in efficacy with later positioning of lacosamide from 100 to 20%. The practical advantage of intravenous lacosamide compared to levetiracetam is the direct injection of the solution without further dilution. First reports on intravenous brivaracetam in status epilepticus are emerging, but patient numbers are too small to draw any reliable conclusions [96].
The “Established Status Epilepticus Treatment Trial” is a randomized, blinded, multicenter study currently comparing efficacy of intravenous fosphenytoin, levetiracetam, and valproic acid in patients with benzodiazepine-refractory status epilepticus [97]. This trial started recruitment in 2015 and is expected to be completed at the end of 2019 with almost 800 patients included. If these objectives will be achieved, high-level evidence would be available for second-line drugs in benzodiazepine-refractory status epilepticus.
In summary, randomized controlled trials have demonstrated with sufficient power that 8-mg intravenous lorazepam (0.1 mg/kg in a patient of 80 kg body weight), 1 mg intravenous clonazepam (0.0125 mg/kg) and—in patients without established venous access at randomization—10 mg intramuscular midazolam (0.125 mg/kg) are efficacious first-line treatment options for generalized convulsive status epilepticus. Intravenous diazepam has only been shown to be as successful as lorazepam if combined with phenytoin [2]. Thus, current European and North American treatment guidelines recommend intravenous lorazepam as the benzodiazepine of choice for first-line treatment in generalized convulsive status epilepticus [98, 99]. As level of evidence for the best second-line anticonvulsant is very low, guidelines recommend use of one of the established available intravenous drugs such as levetiracetam, phenytoin, or valproic acid. Unfortunately, specific randomized controlled trials on first-line treatment of complex focal status epilepticus so far have not been performed, though this clinical form of status epilepticus is the most common [100]. Thus, current guidelines extrapolate the treatment data from trials on generalized convulsive status epilepticus and recommend intravenous lorazepam also in complex focal status epilepticus. If necessary, the same second-line agents as in generalized convulsive status epilepticus are advised [98, 99].
4.3 Treatment Concepts in Refractory Status Epilepticus
Intravenous treatment with a benzodiazepine and a second-line anticonvulsant each in adequate doses, results in cessation of clinical seizure activity in 60% of cases. If seizures continue, status epilepticus is defined as being refractory [99]. At that point, the chance for seizure termination by another non-anesthetizing anticonvulsant is 2% [2].
While evidence on efficacy of first-line anticonvulsants is sufficient and on efficacy of second-line anticonvulsants is weak, evidence on treatment of refractory and super-refractory status epilepticus is almost absent. In the following, we summarize the available findings which are generally derived from uncontrolled prospective studies or retrospective case series.
4.3.1 Refractory Complex Focal Status Epilepticus
The aggressiveness of anticonvulsant treatment of complex focal status epilepticus depends on the estimated risk for acute complications and even more on that for clinical, i.e. cognitive and neurological, long-term consequences. These issues have been discussed above in Sect. 3.
As a general rule, ongoing complex focal status epilepticus itself, i.e. beyond the underlying brain disorder, is unlikely to cause acute complications or significant long-term consequences. Therefore, after failure of a first-line benzodiazepine and a second-line anticonvulsant, rapid treatment escalation with administration of intravenous continuous anesthetic drugs is generally not warranted. Possible complications of treatment—such as ventilator-associated pneumonia, arterial hypotension requiring administration of catecholamines, immunosuppression [101, 102]—may be more hazardous than prolonged non-convulsive seizure activity. Independently from the clinical form of status epilepticus and from confounders such as seizure duration and critical medical conditions, use of anesthetic drugs was associated with higher infection rates and increased mortality [103].
Instead, the entire armamentarium of intravenous non-anesthetizing anticonvulsants including brivaracetam, lacosamide, levetiracetam, phenobarbital, phenytoin, and valproate may be used in adequately high doses [104]. In addition to that, proconvulsant trigger factors such as fever, electrolyte disturbances (e.g. hyponatremia), seizure-provoking drugs (e.g. penicillin, theophylline, etc.) should be eliminated or treated themselves. For most non-anesthetizing anticonvulsants, there are no reliable studies specifically reporting efficacy in refractory complex focal status epilepticus. Rather, the reported episodes of status epilepticus are heterogeneous in regard to clinical form and number of anticonvulsants that had been administered prior to the index anticonvulsant. In the following, we discuss the published clinical data on efficacy of individual anticonvulsants which may be administered to patients with complex focal status epilepticus after failure of benzodiazepines and a second-line drug. The studies mentioned below focus on patients with complex focal status epilepticus but some of them also incorporate data on other clinical forms.
Efficacy of intravenous levetiracetam in status epilepticus is favorable, data from a meta-analysis with 10 retro- and prospective studies (n = 234 patients) indicated seizure termination in 44–94% [105]. In a randomized controlled trial, valproic acid (88%) was as successful as phenytoin (84%) to terminate seizures in benzodiazepine-refractory status epilepticus [91]. Fosphenytoin is a water-soluble phenytoin prodrug. This compound can be infused at higher rates (up to 150 mg/min vs phenytoin at 50 mg/min) and is better tolerated [106, 107]. If available, fosphenytoin should be preferred to phenytoin [17]. Specific studies on phenobarbital in refractory complex focal status epilepticus are not available. Efficacy of intravenous lacosamide for status epilepticus was reported in multiple studies, the two largest of which each comprised more than 50 patients. In an observational prospective study with 53 patients, intravenous lacosamide at 400 mg daily was administered in 45% of cases as third- or fourth-line drug, 57% of patients had non-convulsive status epilepticus [108]. EEG-proven overall seizure termination was achieved in 57% of patients (47% seizure termination in those with non-convulsive status epilepticus). The second larger study with 55 patients was retrospective, 78% had non-convulsive status epilepticus, in 58% lacosamide (200 mg loading dose and 200 mg daily maintenance dose) was administered as third or later anticonvulsant [109]. Seizure termination was seen in 71%, in 49% within 24 h of lacosamide infusion. Response to treatment was predicted by a shorter latency from status epilepticus onset to lacosamide administration. Clinical data on brivaracetam in status epilepticus so far are very sparse. One small retrospective case series with 11 patients (7 of those with dyscognitive/complex focal status epilepticus) from two German centers reported cessation of seizure activity within 24 h after brivaracetam administration in three patients (27%) [96]. The median number of previous acute anticonvulsants was 4 and the median duration before initiation of brivaracetam was 5 days.
4.3.1.1 How to Treat Refractory Complex Focal Status Epilepticus?
If pharmacological management is limited to non-anesthetizing anticonvulsants in order to avoid significant sedation and mechanical ventilation, substances that have not already been administered second-line after failure of benzodiazepines should be given. There is neither a rational for which of these drugs should be injected first nor for the question of whether they should be administered sequentially or some of them in parallel. This decision should be made on the basis of each patient’s individual condition. The available data are sufficient for levetiracetam, phenytoin and valproic acid, expanding for lacosamide and at best preliminary for brivaracetam.
If for some reason early or later in the course of refractory complex focal status epilepticus, use of anesthetics is required, then the treatment options and pathways are the same as described in the following subchapter on refractory generalized convulsive/subtle status epilepticus.
4.3.2 Refractory Generalized Convulsive/Subtle Status Epilepticus
Acute complications including increased mortality and long-term neurological and/or neuropsychological consequences such as memory problems pose significant risks of ongoing generalized convulsive status epilepticus, which clinically evolves to subtle status epilepticus after 1–2 h [23]. To protect the patient as efficiently as possible from these complications and consequences, rapid treatment escalation with use of anesthetic anticonvulsants is urgently required after a benzodiazepine and a second-line anticonvulsant have failed. The general aim is to terminate clinical and EEG seizure activity, i.e. continuous EEG recording is required and recommended in accordant guidelines [110]. The dose of continuous infusion of the anesthetic commonly is titrated against an EEG burst suppression pattern which is maintained for at least 24 h before the anesthetic is tapered [98, 99].
The three most common intravenous anesthetic anticonvulsants are midazolam, propofol and thiopental/pentobarbital. Level of evidence for optimal treatment of refractory generalized convulsive status epilepticus with anesthetics is low.
In a systematic review incorporating 28 studies with 193 patients, barbiturates compared to midazolam and propofol were significantly more successful in suppressing clinical or electrographic ongoing seizure activity [111]. This finding should be interpreted with caution as the titration aim of the anesthetic was “EEG background suppression” in 96% of patients treated with pentobarbital, in 38% administered propofol, and in no patient who was given midazolam. Overall mortality was approximately 50%, with no significant difference between the anesthetic compounds used.
The first-ever randomized trial on the use of anesthetics in refractory status epilepticus compared efficacy and safety of barbiturates (22% success rate) and propofol (43%) [112]. After bolus administration, both anesthetics had rapidly been titrated to an EEG burst suppression pattern maintained for 36–48 h. In that study, intubation time in survivors was significantly longer in those treated with a barbiturate (13.5 days, median) compared to patients treated with propofol (4 days). This difference likely is explained by the longer elimination half-life and thus sedating effect of highly lipophilic barbiturates. After 3 years of enrollment, only 24 patients of 150 needed—following the power analysis—were recruited, although multiple centers in Europe and the USA were involved. This worthwhile attempt underlines the difficulties of conducting randomized controlled trials on refractory status epilepticus.
Further data on the three anesthetic compounds are derived from retrospective or small observational studies, relevant findings are summarized below.
A retrospective study assessed 33 episodes of refractory status epilepticus which were treated with continuous intravenous midazolam [113]. The mean loading dose was 0.19 mg/kg with an infusion rate at 0.22 mg/kg/h. Initially, seizures were stopped clinically and electroencephalographically in 27 out of 33 episodes (82%), but in 56% breakthrough seizures occurred.
Some years later, the same group from Columbia University in New York (USA) had changed their treatment regimen of refractory status epilepticus using higher doses of midazolam with a suggested peak dose of 2.9 mg/kg/h, eventually the median maximum infusion rate was 0.4 mg/kg/h [interquartile range (IQR) 0.2, 1.0] [114]. Comparison of this higher infusion rate to the previously used lower dose with a suggested peak dose of 0.4 mg/kg/h (median maximum rate of 0.2 mg/kg/h; IQR 0.1, 0.3) demonstrated significantly reduced seizure recurrence within 48 h of discontinuation, and lower mortality.
Another retrospective study compared 19 patients treated with midazolam to 14 patients administered thiopental. Efficacy to control refractory status epilepticus did not differ between groups (63 vs 64%), but adverse events were seen significantly more often with thiopental infusion [115].
In a prospective observational study from Finland, midazolam anesthesia was induced in 19 patients with a bolus of 0.2 mg/kg followed by continuous infusion at a starting rate of 1 μg/kg/min (i.e. 0.06 mg/kg/h) [116]. Infusion rate needed to be increased to a median of 8 μg/kg/min (i.e. 0.48 mg/kg/h) in order to suppress clinical status epilepticus. The study is limited by the fact that midazolam treatment was not controlled for with continuous EEG recording. Status epilepticus was terminated in all but one patient, no patient developed pressor-requiring arterial hypotension or other important adverse events.
In a prospective observational study, propofol anesthesia was administered to 10 patients with a bolus of 2–3 mg/kg, and additional boluses of 1–2 mg/kg were given until a burst-suppression EEG pattern was achieved [117]. Thereafter, an infusion of 4 mg/kg/h was initiated; however, the maintenance of continuous burst suppression was difficult requiring incremental doses of propofol with a median maximum infusion rate of 9.5 mg/kg/h. The anesthetic was tapered after 12 h of a sufficient burst suppression pattern, status epilepticus recurred in three patients. Propofol infusion syndrome, i.e. cardiac failure, severe metabolic acidosis, rhabdomyolysis, and renal failure [118], was not reported in any patient of this series. In general, one should be cautious when propofol treatment at a dose of more than 5 mg/kg/h [119] and for more than 48 h [120] is required. Screening patients at risk for propofol infusion syndrome with creatine kinase, lactate and triglycerides may be considered [121]. The key advantage of propofol compared to thiopental was the fast recovery from anesthesia due to short elimination half-time, ventilator and intensive care treatment was only half as long as in a previous similar study with thiopental [122].
In a prospective observational study, thiopental was administered in 10 patients with an initial bolus of 5 mg/kg and subsequent boluses of 1–2 mg/kg to achieve an EEG burst-suppression pattern [122]. The continuous infusion rate was initiated at 5 mg/kg/h and had to be increased to a median of 7 mg/kg/h to maintain the burst-suppression pattern. No patients had a recurrence of epileptic seizure activity following tapering of thiopental after 12 h burst suppression. Decreased arterial pressure required catecholamines in 4 of the 10 patients. Nine patients were treated with antibiotics due to infection indicating the immunosuppressive risk of continuous high-dose thiopental anesthesia. Immunosuppression may put ventilated patients at significant risk of developing pneumonia and even sepsis [101, 102].
4.3.2.1 How to Treat Refractory Generalized Convulsive Status Epilepticus?
This condition is potentially life threatening, therefore continuous intravenous anesthetics have to be administered after failure of a first-line benzodiazepine and a second-line non-anesthetizing anticonvulsant. The drugs of choice are midazolam, propofol, and thiopental/pentobarbital. However, the available data do not allow to favor one of those compounds, a recent Cochrane analysis called for an adequately powered randomized controlled trial [123].
By March 2013, an online multinational registry had been established in which neurologists or intensivists were asked to enter data of consecutive patients with refractory status epilepticus. An interim analysis published in 2015 reported that 488 cases from 44 different countries had been collected [124]. Most of the patients had no history of epilepsy and etiology was unknown. Interestingly, the most widely used anesthetic was midazolam (59%), followed by propofol (32%) and barbiturates (8%). Status epilepticus was terminated in 74% of cases, but in most patients more than one anesthetic had to be administered to achieve this goal.
In summary, the anesthetics midazolam, propofol and thiopental/pentobarbital seem to exhibit some anti-seizure effect in refractory generalized convulsive status epilepticus and should be administered in this condition. It is unclear which of those drugs is best to start with and if combinations of these anesthetics make sense. Randomized controlled trials comparing efficacy of these compounds are urgently needed but obviously very difficult to conduct. Among other explanations, this may be due to the heterogeneity of status epilepticus in regard to etiology, severity and patients’ age.
4.4 Super-Refractory Status Epilepticus
If seizures continue or recur after treatment with anesthetics titrated against an EEG burst-suppression pattern for more than 24 h, status epilepticus nowadays is termed “super-refractory” [20]. Prior to that, the term ‘malignant status epilepticus’ had been coined [5]. In the following, treatment options after failure of the anesthetics midazolam, propofol and/or thiopental/pentobarbital are reported, all of which have a very low level of evidence or are just anecdotal.
4.4.1 Pharmacological Treatments
4.4.1.1 Barbiturates
Even after failure of anesthetics, high-dose barbiturates may be efficacious to terminate—then super-refractory—status epilepticus.
A retrospective study identified 31 out of 147 patients with refractory status epilepticus to fulfill the criteria of super-refractory status epilepticus [6]. Patients with super-refractory status epilepticus were significantly younger and significantly more often had encephalitis as an etiological underlying condition compared to those with status epilepticus responding to anesthetics. Interestingly, these variables exactly confirm those we had identified previously in our study delineating malignant or super-refractory status epilepticus [5]. Only eight out of these 31 patients (26%) had a history of epilepsy. Twenty-nine patients had midazolam as first anesthetic, 13 of whom were then administered propofol; two had propofol as first anesthetic. Median duration of status epilepticus was 6.5 days prior to initiating continuous infusion of pentobarbital. A maintenance dose of 0.5 to 1.7 mg/kg/h was sufficient to maintain an EEG burst-suppression pattern in two-thirds of patients, but rate increases of up to 2.0–3.7 mg/kg/h were necessary for the other one-third. After pentobarbital infusion for a median of 6 days, status epilepticus was successfully terminated in 90% of patients. On tapering pentobarbital, withdrawal seizures were observed in 15 out of 31 patients, controlled by intravenous phenobarbital in 12 patients (80%). Adverse events included ventilator-associated pneumonia (32%), hypotension requiring pressors (32%), urinary tract infection (13%), deep venous thrombosis (10%), and ileus (10%).
Another small retrospective series reported 10 patients with super-refractory status epilepticus in all cases, presumably caused by encephalitis [125]. The patients were treated with continuous intravenous phenobarbital at high doses between 0.75 and 4 mg/kg/h, maximal serum concentrations were between 80 and 350 mg/L (median 152 mg/L). After 25 days, this regimen was initially successful in eight patients, five had favorable outcome, two had withdrawal seizures on tapering, and one died of septic shock during phenobarbital treatment. In the other two patients, high-dose phenobarbital did not have any anti-seizure effect and other compounds had to be introduced. Systemic infection occurred in all 10 patients, including pneumonia (5), urinary tract infection (4), fungal infection (2), and venous line infection (2), either alone or in combination. Three patients had sepsis after fungal infection or bacterial pneumonia. Seven patients developed pressor-requiring arterial hypotension, and four had ileus.
In summary, both intravenous pentobarbital and high-dose phenobarbital administered for days or weeks have been shown to exhibit some potential to terminate seizure activity in super-refractory status epilepticus after other anesthetics such as midazolam and propofol had failed. The risks include immunosuppressive adverse effects which facilitate systemic infections or even sepsis.
4.4.1.2 Ketamine
Three retrospective studies report more than 150 patients with difficult-to-treat status epilepticus who were administered ketamine (details are given in Table 1). In patients without anoxic encephalopathy (n = 135), super-refractory status epilepticus was terminated in 15 out of 53 patients (28.3%) [126], in 18 out of 28 patients (64.3%) [127], and in 52 out of 54 patients (96.3%) [128]. In the latter study, excellent response rates may be explained by co-administration of propofol in all patients. When this study is not considered, efficacy rate of ketamine in super-refractory status epilepticus in the two other studies is still 40.3% (33 out of 81 patients with non-anoxic etiology) [126, 127]. One of the clinical advantages of ketamine is the lack of cardiorespiratory depression [129].
In summary, among all anesthetic anticonvulsants available, ketamine has a unique mechanism of action that becomes more relevant with ongoing seizure activity due to increased externalization of post-synaptic NMDA receptors. In super-refractory status epilepticus, ketamine should be co-administered to GABAergic compounds, the latter are needed to counteract possible neurotoxic effects of the NMDA receptor antagonist.
4.4.1.3 Inhalational Anesthetics
In seven patients with super-refractory status epilepticus, the inhaled substances isoflurane and desflurane in end-tidal concentrations of 1.2–5% resulted in an EEG burst-suppression pattern and thus terminated seizure activity within minutes [130]. The inhalational anesthetics had been administered for more than 10 days.
Another small retrospective study assessed efficacy and safety of isoflurane which was administered to control status epilepticus on 11 occasions in nine patients [131]. The volatile anesthetic was administered for 1–55 h, titration towards a burst-suppression pattern on EEG terminated seizures in all patients. In all patients, arterial hypotension occurred requiring blood pressure support with intravenous fluids and/or pressor infusions. Upon tapering of isoflurane, seizure activity recurred in 8 out of 11 episodes.
In a systematic literature review including the two studies mentioned above, 28 adult patients treated with inhalational anesthetics for super-refractory status epilepticus were identified [132]. Seizure control was reached in all but two patients (93%). In most cases, isoflurane was administered. Arterial hypotension was the only complication reported.
In summary, volatile anesthetics seem to have the capacity to suppress seizure activity in super-refractory status epilepticus, but with tapering, seizure recurrence may become a problem. Given the technical difficulties concerning prolonged treatment with volatile drugs and the sparse clinical experience, isoflurane may be administered in selected cases only. In this field, further data are needed.
4.4.1.4 Non-intravenous Anticonvulsant Drugs
A number of “classical” anticonvulsant drugs which are not available in intravenous formulations have been reported for administration in super-refractory status epilepticus. In general, these are case reports or very small retrospective case series. Beyond the limitation of reporting bias, the possibility of spontaneous cessation of seizure activity and the effects of co-administered intravenous anticonvulsants have to be considered.
Perampanel is an antagonist at the alpha-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid (AMPA) receptor. Its anticonvulsant efficacy for status epilepticus has been assessed in the lithium-pilocarpine model [133]. Perampanel at a dose of 8 mg/kg terminated seizures in 6 out of 6 rats after both 10 and 30 min of status epilepticus. Co-administration of diazepam at 5 mg/kg allowed to reduce the dose of perampanel to 1 mg/kg in order to terminate seizure activity in a set of 9 out of 9 rats after 30 min of status epilepticus. These experimental data indicate the supporting therapeutic potential of perampanel and its synergy if co-administered to a benzodiazepine in difficult-to-treat status epilepticus. Two retrospective studies reported 22 episodes of at least refractory status epilepticus treated with perampanel. In an Austrian series, 12 patients received perampanel administered per nasogastric tube [134]. Perampanel was deployed after failure of a median of four other anticonvulsants and after a median of 1.5 days. Only 2 of 12 patients had some kind of clinical and EEG improvement after 48–60 h. The median initial dose was 4 mg which was titrated up to a median of 12 mg. No relevant adverse effects were reported. In the second study from Germany, 10 episodes with perampanel for difficult-to-treat status epilepticus were reported [135]. This anticonvulsant was administered after failure of a mean of five previous drugs. Most patients received a dose of 6 mg per day, termination of seizure activity was observed in 4 of 10 episodes.
In a systematic review on topiramate with individual patient data analysis, 35 patients from 4 studies were identified, only 6 of which had super-refractory status epilepticus [136]. In five of those six patients, topiramate was administered as the last anticonvulsant, seizure activity was terminated in four cases.
Oxcarbazepine was identified for treatment of difficult-to-treat status epilepticus in 13 patients [137]. This anticonvulsant was initiated as third or later agent in almost all patients after a median latency of 81 h, the median maximum daily dose was 1.800 mg. Oxcarbazepine was the last drug before termination of seizure activity in 8 out of 13 patients. In three patients, relevant hyponatremia (< 125 mmol/L) was reported.
The efficacy of oral pregabalin administration was reported in one retrospective study [138]. Most patients had focal status epilepticus, and 450 mg pregabalin terminated seizure activity in 5 of 11 patients, in another 3, this compound had a possible response; no adverse events were reported.
No reliable clinical reports were found for carbamazepine, eslicarbazepine acetate, lamotrigine, and zonisamide. In a model of secondarily generalized convulsive status epilepticus in rats (cortical cobalt lesions induced by administration of homocysteine thiolactone), the efficacy of lamotrigine had been compared to that of phenytoin [139]. Phenytoin controlled generalized tonic-clonic seizures with a median dose of 100.5 mg/kg (16.0 mg/L in serum), but lamotrigine was ineffective at doses ranging from 10 to 100 mg/kg, with serum drug concentrations between 2.5 and 43.5 mg/L.
In summary, non-intravenous anticonvulsants may be used as adjunct in in super-refractory status epilepticus but level of evidence for efficacy is very low.
4.4.1.5 Immunomodulation
Two retrospective studies have analyzed clinical variables independently associated with super-refractory status epilepticus compared to refractory status epilepticus responding to anesthetic anticonvulsants [5, 6]. Interestingly, both studies identified the same predictors, younger age and encephalitis as etiology. At the beginning of this century, such cases of encephalitis were thought to be of viral origin without proof for a biological agent or of unknown cause at all [5]. Later, it became evident that encephalitis underlying exactly these cases of super-refractory status epilepticus was associated and likely caused by anti-NMDA receptor antibodies [140]. In a retrospective European multicenter survey, 7 centers provided detailed data on 13 adult patients with antibody-mediated status epilepticus [141]. All but one patient were female, age at onset was at a median of 25 years with wide range (17–69 years). The duration of the disease was also highly variable (2 h to 12 years, median: 2 months). Eight out of 13 patients were diagnosed with anti-NMDA receptor encephalitis. Interestingly, no specific treatment regimen—either anticonvulsant or immunomodulatory—was found to be clearly superior. Three elderly patients had died, but the other patients recovered almost completely within the following 2 years. A retrospective review of patients with new-onset refractory status epilepticus revealed that autoimmune encephalitis is the most commonly identified cause [142].
The immunomodulatory treatment in autoimmune-mediated status epilepticus conforms to that of antibody-mediated encephalitis. This comprehensive topic is beyond the scope of this review article, we refer to accordant publications [143].
4.4.1.6 Perspectives
In the last years or even decades, there has been little but at least some progress in the development of novel treatment approaches in status epilepticus in general and in refractory and super-refractory status epilepticus in particular. An emerging concept may be the co-administration of substances that enhance efficacy of well-known substances.
The loop diuretic bumetanide is an inhibitor of the Cl− intruding Na+–K+–Cl−-cotransporter NKCC1, which reduces intraneuronal Cl−. In three experimental models of status epilepticus, the kainate and the lithium-pilocarpine model as well as model of sustained electrical stimulation of the basolateral amygdala, bumetanide was ineffective to terminate seizure activity [144]. But bumetanide potentiated the anticonvulsant effect of low doses of phenobarbital. However, higher doses of phenobarbital, particularly in combination with diazepam, were more effective to terminate seizure activity than co-administration of bumetanide and phenobarbital. Clinical data confirm these negative experimental findings. An open-label, dose finding, and feasibility Phase 1/2 trial on newborn babies with severe seizures due to hypoxic ischemic encephalopathy demonstrated that bumetanide at four different doses was not more efficient than phenobarbital [145]. In addition, bumetanide increased the risk of hearing loss.
Specific neurosteroids have the capacity to allosterically modulate activity of GABAA receptors via distinct binding sites on this receptor [146]. Allopregnanolone, which is a natural metabolite of progesterone, allosterically enhances currents at GABAA receptors [147]. In a multicenter, Phase 1/2 study in patients with super-refractory status epilepticus, safety and tolerability of brexanolone (which is another name for allopregnanolone) was assessed [148]. A secondary objective was open-label evaluation of efficacy of brexanolone during and after weaning of the anesthetic anticonvulsant administrated as third-line agent. After 48 h of brexanolone infusion, anesthetic anticonvulsants were withdrawn while brexanolone was continued. In this pilot study, 25 patients were administered brexanolone. No serious adverse events occurred that could have been attributed to the study drug. In 22 patients, the anesthetic anticonvulsants were tapered, and in 16 of these patients (73%), seizure activity did not recur within 5 days of weaning the anesthetic anticonvulsant. These preliminary data indicated that allopregnanolone/brexanolone seems to be a promising compound in super-refractory status epilepticus. However, a randomized, double-blind, placebo-controlled Phase 3 study did not meet the primary endpoint, i.e. success in weaning of third-line anesthetic agents and remaining free of status epilepticus with brexanolone versus placebo (43.9 vs 42.4%; p = 0.8775) when added to standard-of-care [149]. In summary, the neurosteroid brexanolone did not prove to be efficient in super-refractory status epilepticus after failure of GABAergic anesthetic anticonvulsants when compared to placebo.
4.4.2 Non-pharmacological Treatment Approaches
Though slightly beyond the scope of this review article, some non-pharmacological treatment approaches in super-refractory status epilepticus are summarized below. Again, data are mostly obtained from small case series with low levels of evidence.
4.4.2.1 Ketogenic Diet
Ketogenic diet is a strict low-carb diet that results in elevated free fatty acids, these lead to production of ketone bodies and increased concentrations of polyunsaturated fatty acids in the brain [150]. The exact mechanisms of action for the anticonvulsant properties of ketogenic diet are elusive, it likely works through multiple mechanisms. Eventually, neurons are hyperpolarized by keton bodies and thus neuronal excitability is decreased [151].
In 1925, the first larger study on 37 patients with epilepsy assessed efficacy of ketogenic diet, 19 patients (51%) were seizure-free after a follow-up of 4–12 months [152].
In a rodent model of pilocarpine-induced status epilepticus, pretreatment with ketogenic diet resulted in a delayed onset of continuous seizure activity [153]. The effect of ketogenic diet administered in experimental animals with established status epilepticus has not been assessed so far.
A retrospective case series on ketogenic diet in patients with super-refractory status epilepticus identified 10 adult patients from 4 centers [154]. In 7 of the 10 patients, encephalitis was the underlying etiology confirming the previously reported strong link between encephalitis and super-refractory status epilepticus [5, 6]. Status epilepticus had lasted a median of 21.5 days, before ketogenic diet was started. Nine out of 10 patients achieved ketosis, in all those patients, seizure activity was stopped after a median of 3 days. Three patients had transient acidosis and hypertriglyceridemia, but no other adverse events were reported.
These promising findings have led to conduct a multicenter Phase 1/2 study on ketogenic diet for adult patients with super-refractory status epilepticus [155]. Fifteen patients were administered classic ketogenic diet via gastrostomy tube. Median duration of status epilepticus before ketogenic was initiated was 10 days, all patients were in ketosis after a median of 2 days. In 11 of 14 patients who completed treatment with ketogenic diet, super-refractory status epilepticus resolved (79%). Reported adverse events comprised metabolic acidosis, hyperlipidemia, constipation, hypoglycemia, hyponatremia, and weight loss.
In summary, administration of ketogenic diet is feasible and seems safe in super-refractory status epilepticus, data from a retrospective study and from a prospective Phase 1/2 trial point to favorable efficacy. A randomized, placebo-controlled trial is warranted.
4.4.2.2 Hypothermia
The anticonvulsant effect of decreased body temperature may be explained by multiple mechanisms including presynaptic alterations with marked reduction of excitatory transmitter release [156, 157], alteration of postsynaptic voltage-gated channels [158], and disturbances of membrane properties and ion pumps [159].
In experimental models of status epilepticus, hypothermia has been shown to have anticonvulsant properties. In rodents with status epilepticus induced by kainic acid, lowering body temperature to 28 °C stopped seizures in half of the animals, body temperature of 23 °C terminated seizure activity in all animals [160]. In the model system of SSSE after perforant path stimulation, cooling to 29 °C body temperature significantly reduced the number and severity of motor seizures but did not alter electrographic seizure activity [161]. With rewarming, motor seizure recurred. Using the same model, 10 rats were cooled down to 20 °C, in four of those rats, seizures were completely suppressed and did not recur with warming [162].
A systematic review identified 13 studies with 40 patients with difficult-to-treat status epilepticus who underwent hypothermia. In general, the target body temperature was 33 °C, which was sustained for a median of 48 h. Seizure termination was reported in 25 of 40 patients (62.5%) [163]. This surprisingly favorable result may be limited by some reporting bias. Frequent adverse events were deep venous thrombosis, coagulopathy and infections.
In a randomized controlled trial, 268 patients with generalized convulsive status epilepticus either were cooled down to 33 °C for 24 h followed by another 24 h of rewarming in addition to standard treatment or they received standard treatment alone [164]. The primary outcome was absence of functional impairment after 90 min, but the study did not demonstrate differences between groups. One of the secondary outcomes was progression to EEG-confirmed status epilepticus, this was seen significantly less often with hypothermia than without. Rate of progression to refractory and super-refractory status epilepticus was not influenced by hypothermia. This trial demonstrated some anticonvulsant effects of cooling, but the data refer to early phases of status epilepticus and cannot be translated to super-refractory status epilepticus.
In summary, there are some hints for anticonvulsant effects of hypothermia but specific data on super-refractory status epilepticus are currently not available.
4.4.2.3 Epilepsy Surgery
In patients with intractable focal epilepsy, resective epilepsy surgery aims to completely remove the epileptogenic zone and to render the patient seizure-free. If pharmacoresistant super-refractory status epilepticus can be attributed to a circumscribed brain region, resection of this structure may terminate ongoing seizure activity.
The largest cohort of adult patients with super-refractory status epilepticus who underwent epilepsy surgery reported nine individuals [165]. Resections were performed after 10–54 days of status epilepticus and were guided by electrocorticography. Five out of eight survived patients were seizure-free after epilepsy surgery.
In addition to this series, there are some case reports on epilepsy surgery in difficult-to-treat status epilepticus.
In summary, the decision to perform epilepsy surgery in super-refractory status epilepticus is highly individualized. If the seizure focus can be identified and is remote from eloquent brain structures, resection may be considered as ultima ratio.
4.4.3 How to Treat Super-Refractory Status Epilepticus?
When status epilepticus does not respond to the intravenous GABAergic anesthetic anticonvulsants midazolam, propofol, or thiopental/pentobarbital and is thus defined as super-refractory, treatment becomes even more challenging.
The most promising compound is the NMDA-receptor antagonist ketamine while the GABAA receptor modulator allopregnanolone/brexanolone so far has failed to prove efficacy. For the estimate of the efficacy of ketamine, only retrospective data are available, and prospective studies are urgently required.
On the non-pharmacological side, ketogenic diet also seems to be promising, retro- and prospective data indicate strong efficacy if ketosis is achieved. Hypothermia seems to work in animal models, but so far, no clinical data have demonstrated efficacy.
All other pharmacological and non-pharmacological treatment approaches may be applied individually on a trial and error basis.
5 Conclusion
Evidence for pharmacological treatment of refractory and super-refractory status epilepticus is very low. It is unclear what is the optimal non-anesthetizing anticonvulsant in complex focal status epilepticus and what is the optimal anesthetic anticonvulsant in generalized convulsive status epilepticus. If status epilepticus becomes super-refractory, further treatment is even more unclear. Promising approaches are the NMDA-receptor antagonist ketamine, and, on the non-pharmacological side, ketogenic diet. Randomized controlled trials for treatment of refractory and super-refractory status epilepticus are desirable, but difficult to conduct; at first, large, multicenter registries would be an acceptable alternative.
References
Neligan A, Shorvon SD. Frequency and prognosis of convulsive status epilepticus of different causes: a systematic review. Arch Neurol. 2010;67:931–40.
Treiman DM, Meyers PD, Walton NY, Collins JF, Colling C, Rowan AJ, Handforth A, Faught E, Calabrese VP, Uthman BM, Ramsay RE, Mamdani MB. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339:792–8.
Rossetti AO, Logroscino G, Bromfield EB. Refractory status epilepticus: effect of treatment aggressiveness on prognosis. Arch Neurol. 2005;62:1698–702.
Holtkamp M, Othman J, Buchheim K, Meierkord H. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry. 2005;76:534–9.
Holtkamp M, Othman J, Buchheim K, Masuhr F, Schielke E, Meierkord H. A “malignant” variant of status epilepticus. Arch Neurol. 2005;62:1428–31.
Pugin D, Foreman B, De Marchis GM, Fernandez A, Schmidt JM, Czeisler BM, Mayer SA, Agarwal S, Lesch C, Lantigua H, Claassen J. Is pentobarbital safe and efficacious in the treatment of super-refractory status epilepticus: a cohort study. Crit Care. 2014;18:R103.
Strzelczyk A, Ansorge S, Hapfelmeier J, Bonthapally V, Erder MH, Rosenow F. Costs, length of stay, and mortality of super-refractory status epilepticus: a population-based study from Germany. Epilepsia. 2017;58:1533–41.
Kantanen AM, Reinikainen M, Parviainen I, Ruokonen E, Ala-Peijari M, Backlund T, Koskenkari J, Laitio R, Kalviainen R. Incidence and mortality of super-refractory status epilepticus in adults. Epilepsy Behav. 2015;49:131–4.
Ferlisi M, Shorvon S. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain. 2012;135:2314–28.
Penberthy LT, Towne A, Garnett LK, Perlin JB, DeLorenzo RJ. Estimating the economic burden of status epilepticus to the health care system. Seizure. 2005;14:46–51.
Beg JM, Anderson TD, Francis K, Meckley LM, Fitzhenry D, Foster T, Sukhtankar S, Kanes SJ, Moura LM. Burden of illness for super-refractory status epilepticus patients. J Med Econ. 2017;20:45–53.
Pichler M, Hocker S. Management of status epilepticus. Handb Clin Neurol. 2017;140:131–51.
Trinka E, Brigo F, Shorvon S. Recent advances in status epilepticus. Curr Opin Neurol. 2016;29:189–98.
Betjemann JP, Lowenstein DH. Status epilepticus in adults. Lancet Neurol. 2015;14:615–24.
Rossetti AO, Lowenstein DH. Management of refractory status epilepticus in adults: still more questions than answers. Lancet Neurol. 2011;10:922–30.
Trinka E, Hofler J, Leitinger M, Brigo F. Pharmacotherapy for status epilepticus. Drugs. 2015;75:1499–521.
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, Bare M, Bleck T, Dodson WE, Garrity L, Jagoda A, Lowenstein D, Pellock J, Riviello J, Sloan E, Treiman DM. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016;16:48–61.
Verrotti A, Ambrosi M, Pavone P, Striano P. Pediatric status epilepticus: improved management with new drug therapies? Expert Opin Pharmacother. 2017;18:789–98.
Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, Shorvon S, Lowenstein DH. A definition and classification of status epilepticus—report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56:1515–23.
Shorvon S. Super-refractory status epilepticus: an approach to therapy in this difficult clinical situation. Epilepsia. 2011;52(Suppl 8):53–6.
Walton NY. Systemic effects of generalized convulsive status epilepticus. Epilepsia. 1993;34(Suppl 1):S54–8.
DeLorenzo RJ, Garnett LK, Towne AR, Waterhouse EJ, Boggs JG, Morton L, Choudhry MA, Barnes T, Ko D. Comparison of status epilepticus with prolonged seizure episodes lasting from 10 to 29 minutes. Epilepsia. 1999;40:164–9.
Treiman DM, Walton NY, Kendrick C. A progressive sequence of electroencephalographic changes during generalized convulsive status epilepticus. Epilepsy Res. 1990;5:49–60.
Meierkord H, Holtkamp M. Non-convulsive status epilepticus in adults: clinical forms and treatment. Lancet Neurol. 2007;6:329–39.
Bauer G, Gotwald T, Dobesberger J, Embacher N, Felber S, Bauer R, Seppi K, Walser G, Trinka E, Poewe W. Transient and permanent magnetic resonance imaging abnormalities after complex partial status epilepticus. Epilepsy Behav. 2006;8:666–71.
DeGiorgio CM, Gott PS, Rabinowicz AL, Heck CN, Smith TD, Correale JD. Neuron-specific enolase, a marker of acute neuronal injury, is increased in complex partial status epilepticus. Epilepsia. 1996;37:606–9.
DeGiorgio CM, Heck CN, Rabinowicz AL, Gott PS, Smith T, Correale J. Serum neuron-specific enolase in the major subtypes of status epilepticus. Neurology. 1999;52:746–9.
Kucken AM, Teissere JA, Seffinga-Clark J, Wagner DA, Czajkowski C. Structural requirements for imidazobenzodiazepine binding to GABA(A) receptors. Mol Pharmacol. 2003;63:289–96.
Macdonald RL. Mechanisms of anticonvulsant drug action. In: Pedley TA, Meldrum BS, editors. Recent advances in epilepsy I. Edinburgh: Churchill Livingstone; 1983. p. 1–23.
Barker J, Owen DG. Electrophysiological pharmacology of GABA and diazepam in cultured CNS neurons. In: Olsen RW, Venter JC, editors. Benzodiazepine/GABA receptors and chloride channels: structural and functional properties. New York: Alan R. Liss; 1986. p. 135–65.
Porter RJ, Dhir A, Macdonald RL, Rogawski MA. Mechanisms of action of antiseizure drugs. Handb Clin Neurol. 2012;108:663–81.
Mazarati AM, Baldwin RA, Sankar R, Wasterlain CG. Time-dependent decrease in the effectiveness of antiepileptic drugs during the course of self-sustaining status epilepticus. Brain Res. 1998;814:179–85.
Walton NY, Treiman DM. Lorazepam treatment of experimental status epilepticus in the rat: relevance to clinical practice. Neurology. 1990;40:990–4.
Celesia GG, Booker HE, Sato S. Brain and serum concentrations of diazepam in experimental epilepsy. Epilepsia. 1974;15:417–25.
Lowenstein DH, Alldredge BK. Status epilepticus. N Engl J Med. 1998;338:970–6.
Milovanovic JR, Jankovic SM, Pejcic A, Milosavljevic M, Opancina V, Radonjic V, Protrka Z, Kostic M. Evaluation of brivaracetam: a new drug to treat epilepsy. Expert Opin Pharmacother. 2017;18:1381–9.
Klitgaard H, Matagne A, Nicolas JM, Gillard M, Lamberty Y, De RM, Kaminski RM, Leclercq K, Niespodziany I, Wolff C, Wood M, Hannestad J, Kervyn S, Kenda B. Brivaracetam: rationale for discovery and preclinical profile of a selective SV2A ligand for epilepsy treatment. Epilepsia. 2016;57:538–48.
Niquet J, Suchomelova L, Thompson K, Klitgaard H, Matagne A, Wasterlain C. Acute and long-term effects of brivaracetam and brivaracetam–diazepam combinations in an experimental model of status epilepticus. Epilepsia. 2017;58:1199–207.
Klein P, Biton V, Dilley D, Barnes M, Schiemann J, Lu S. Safety and tolerability of adjunctive brivaracetam as intravenous infusion or bolus in patients with epilepsy. Epilepsia. 2016;57:1130–8.
Campagna JA, Miller KW, Forman SA. Mechanisms of actions of inhaled anesthetics. N Engl J Med. 2003;348:2110–24.
Grasshoff C, Antkowiak B. Effects of isoflurane and enflurane on GABAA and glycine receptors contribute equally to depressant actions on spinal ventral horn neurones in rats. Br J Anaesth. 2006;97:687–94.
Murao K, Shingu K, Tsushima K, Takahira K, Ikeda S, Matsumoto H, Nakao S, Asai T. The anticonvulsant effects of volatile anesthetics on penicillin-induced status epilepticus in cats. Anesth Analg. 2000;90:142–7.
Naylor DE, Liu H, Wasterlain CG. Trafficking of GABA(A) receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J Neurosci. 2005;25:7724–33.
Chen JW, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5:246–56.
Walker MC, Fisher A. Mechanisms of antiepileptic drug action. In: Shorvon S, Perucca E, Fish D, Dodson E, editors. The treatment of epilepsy. Oxford: Blackwell Publishing; 2004. p. 96–119.
Dingledine R, Borges K, Bowie D, Traynelis SF. The glutamate receptor ion channels. Pharmacol Rev. 1999;51:7–61.
Borris DJ, Bertram EH, Kapur J. Ketamine controls prolonged status epilepticus. Epilepsy Res. 2000;42:117–22.
Martin BS, Kapur J. A combination of ketamine and diazepam synergistically controls refractory status epilepticus induced by cholinergic stimulation. Epilepsia. 2008;49:248–55.
Niquet J, Baldwin R, Norman K, Suchomelova L, Lumley L, Wasterlain CG. Midazolam-ketamine dual therapy stops cholinergic status epilepticus and reduces Morris water maze deficits. Epilepsia. 2016;57:1406–15.
Rogawski MA, Tofighy A, White HS, Matagne A, Wolff C. Current understanding of the mechanism of action of the antiepileptic drug lacosamide. Epilepsy Res. 2015;110:189–205.
Holtkamp D, Opitz T, Niespodziany I, Wolff C, Beck H. Activity of the anticonvulsant lacosamide in experimental and human epilepsy via selective effects on slow Na+ channel inactivation. Epilepsia. 2017;58:27–41.
Wasterlain CG, Stohr T, Matagne A. The acute and chronic effects of the novel anticonvulsant lacosamide in an experimental model of status epilepticus. Epilepsy Res. 2011;94:10–7.
Fountain NB, Krauss G, Isojarvi J, Dilley D, Doty P, Rudd GD. Safety and tolerability of adjunctive lacosamide intravenous loading dose in lacosamide-naive patients with partial-onset seizures. Epilepsia. 2013;54:58–65.
Li W, Stefan H, Matzen J, Rampp S, Heinze HJ, Schmitt FC. Rapid loading of intravenous lacosamide: efficacy and practicability during presurgical video-EEG monitoring. Epilepsia. 2013;54:75–80.
Lyseng-Williamson KA. Levetiracetam: a review of its use in epilepsy. Drugs. 2011;71:489–514.
Putnam TJ, Merritt HH. Experimental determination of the anticonvulsant properties of some phenyl derivates. Science. 1937;85:525–6.
Everett GM, Richards RK. Comparative anticonvulsant action of 3,5,5,-trimethyloxazolidine-2-4-dione (tridone), dilantin and phenobarbital. J Pharmacol Exp Ther. 1944;1:402–7.
Brown WC, Schiffman DO, Swinyard EA, Goodman LS. Comparative assay of an antiepileptic drugs by psychomotor seizure test and minimal electroshock threshold test. J Pharmacol Exp Ther. 1953;1953(107):273–83.
Barton ME, Klein BD, Wolf HH, White HS. Pharmacological characterization of the 6 Hz psychomotor seizure model of partial epilepsy. Epilepsy Res. 2001;47:217–27.
Mazarati AM, Baldwin R, Klitgaard H, Matagne A, Wasterlain CG. Anticonvulsant effects of levetiracetam and levetiracetam–diazepam combinations in experimental status epilepticus. Epilepsy Res. 2004;58:167–74.
Uges JW, van Huizen MD, Engelsman J, Wilms EB, Touw DJ, Peeters E, Vecht CJ. Safety and pharmacokinetics of intravenous levetiracetam infusion as add-on in status epilepticus. Epilepsia. 2009;50:415–21.
Rogawski MA, Loscher W. The neurobiology of antiepileptic drugs. Nat Rev Neurosci. 2004;5:553–64.
Cossart R, Bernard C, Ben-Ari Y. Multiple facets of GABAergic neurons and synapses: multiple fates of GABA signalling in epilepsies. Trends Neurosci. 2005;28:108–15.
Rogers CJ, Twyman RE, Macdonald RL. Benzodiazepine and beta-carboline regulation of single GABAA receptor channels of mouse spinal neurones in culture. J Physiol. 1994;475:69–82.
Macdonald RL, Olsen RW. GABAA receptor channels. Annu Rev Neurosci. 1994;17:569–602.
Twyman RE, Rogers CJ, Macdonald RL. Differential regulation of gamma-aminobutyric acid receptor channels by diazepam and phenobarbital. Ann Neurol. 1989;25:213–20.
Shorvon SD. Drug treatment of epilepsy in the century of the ILAE: the first 50 years, 1909–1958. Epilepsia. 2009;50(Suppl 3):69–92.
Kumbier E, Haack K. From a hypnotic to an antiepileptic drug—the discovery of the antiepileptic effect of phenobarbital by Alfred Hauptmann. Akt Neurol. 2004;31:302–6.
Hauptmann A. Luminal bei epilepsie. Mnch Med Wochenschr. 1912;59:1907–9.
Hauptmann A. Erfahrungen aus der Behandlung der Epilepsie mit Luminal. Mnch Med Wochenschr. 1919;46:1319–21.
Walton NY, Treiman DM. Phenobarbital treatment of status epilepticus in a rodent model. Epilepsy Res. 1989;4:216–21.
Macdonald RL, Kelly KM. Antiepileptic drug mechanisms of action. Epilepsia. 1995;36(Suppl 2):S2–12.
Kuo CC. A common anticonvulsant binding site for phenytoin, carbamazepine, and lamotrigine in neuronal Na+ channels. Mol Pharmacol. 1998;54:712–21.
Holtkamp M, Meierkord H. Anticonvulsant, antiepileptogenic, and antiictogenic pharmacostrategies. Cell Mol Life Sci. 2007;64:2023–41.
Hara M, Kai Y, Ikemoto Y. Propofol activates GABAA receptor-chloride ionophore complex in dissociated hippocampal pyramidal neurons of the rat. Anesthesiology. 1993;79:781–8.
Adodra S, Hales TG. Potentiation, activation and blockade of GABAA receptors of clonal murine hypothalamic GT1-7 neurones by propofol. Br J Pharmacol. 1995;115:953–60.
Orser BA, Wang LY, Pennefather PS, MacDonald JF. Propofol modulates activation and desensitization of GABAA receptors in cultured murine hippocampal neurons. J Neurosci. 1994;14:7747–60.
Hara M, Kai Y, Ikemoto Y. Enhancement by propofol of the gamma-aminobutyric acidA response in dissociated hippocampal pyramidal neurons of the rat. Anesthesiology. 1994;81:988–94.
Holtkamp M, Tong X, Walker MC. Propofol in subanesthetic doses terminates status epilepticus in a rodent model. Ann Neurol. 2001;49:260–3.
Study RE, Barker JL. Diazepam and (–)-pentobarbital: fluctuation analysis reveals different mechanisms for potentiation of gamma-aminobutyric acid responses in cultured central neurons. Proc Natl Acad Sci USA. 1981;78:7180–4.
Holtkamp M. The anaesthetic and intensive care of status epilepticus. Curr Opin Neurol. 2007;20:188–93.
Godin Y, Heiner L, Mark J, Mandel P. Effects of DI-n-propylacetate, and anticonvulsive compound, on GABA metabolism. J Neurochem. 1969;16:869–73.
Johannessen CU. Mechanisms of action of valproate: a commentatory. Neurochem Int. 2000;37:103–10.
Loscher W. Valproate enhances GABA turnover in the substantia nigra. Brain Res. 1989;501:198–203.
Walton NY, Treiman DM. Valproic acid treatment of experimental status epilepticus. Epilepsy Res. 1992;12:199–205.
Hussein Z, Mukherjee D, Lamm J, Cavanaugh JH, Granneman GR. Pharmacokinetics of valproate after multiple-dose oral and intravenous infusion administration: gastrointestinal-related diurnal variation. J Clin Pharmacol. 1994;34:754–9.
Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S, Gottwald MD, O’Neil N, Neuhaus JM, Segal MR, Lowenstein DH. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–7.
Silbergleit R, Durkalski V, Lowenstein D, Conwit R, Pancioli A, Palesch Y, Barsan W. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med. 2012;366:591–600.
Navarro V, Dagron C, Elie C, Lamhaut L, Demeret S, Urien S, An K, Bolgert F, Treluyer JM, Baulac M, Carli P. Prehospital treatment with levetiracetam plus clonazepam or placebo plus clonazepam in status epilepticus (SAMUKeppra): a randomised, double-blind, phase 3 trial. Lancet Neurol. 2016;15:47–55.
Leppik IE, Derivan AT, Homan RW, Walker J, Ramsay RE, Patrick B. Double-blind study of lorazepam and diazepam in status epilepticus. JAMA. 1983;249:1452–4.
Agarwal P, Kumar N, Chandra R, Gupta G, Antony AR, Garg N. Randomized study of intravenous valproate and phenytoin in status epilepticus. Seizure. 2007;16:527–32.
Chen WB, Gao R, Su YY, Zhao JW, Zhang YZ, Wang L, Ren Y, Fan CQ. Valproate versus diazepam for generalized convulsive status epilepticus: a pilot study. Eur J Neurol. 2011;18:1391–6.
Brigo F, Bragazzi N, Nardone R, Trinka E. Direct and indirect comparison meta-analysis of levetiracetam versus phenytoin or valproate for convulsive status epilepticus. Epilepsy Behav. 2016;64:110–5.
Yasiry Z, Shorvon SD. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepine-resistant convulsive status epilepticus: a meta-analysis of published studies. Seizure. 2014;23:167–74.
Strzelczyk A, Zollner JP, Willems LM, Jost J, Paule E, Schubert-Bast S, Rosenow F, Bauer S. Lacosamide in status epilepticus: systematic review of current evidence. Epilepsia. 2017;58:933–50.
Strzelczyk A, Steinig I, Willems LM, Reif PS, Senft C, Voss M, Gaida B, von Podewils F, Rosenow F. Treatment of refractory and super-refractory status epilepticus with brivaracetam: a cohort study from two German university hospitals. Epilepsy Behav. 2017;70:177–81.
Bleck T, Cock H, Chamberlain J, Cloyd J, Connor J, Elm J, Fountain N, Jones E, Lowenstein D, Shinnar S, Silbergleit R, Treiman D, Trinka E, Kapur J. The established status epilepticus trial 2013. Epilepsia. 2013;54(Suppl 6):89–92.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, Laroche SM, Riviello JJ Jr, Shutter L, Sperling MR, Treiman DM, Vespa PM. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Meierkord H, Boon P, Engelsen B, Gocke K, Shorvon S, Tinuper P, Holtkamp M. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17:348–55.
Knake S, Rosenow F, Vescovi M, Oertel WH, Mueller HH, Wirbatz A, Katsarou N, Hamer HM. Incidence of status epilepticus in adults in Germany: a prospective, population-based study. Epilepsia. 2001;42:714–8.
Ropper AH. Neurological und neurosurgical intensive care. 4th ed. Boston: Lippincott, Williams & Wilkins; 2003.
Lovett EJ III, Alderman J, Munster E, Lundy J. Suppressive effects of thiopental and halothane on specific arms of the immune response. J Surg Oncol. 1980;15:327–34.
Sutter R, Marsch S, Fuhr P, Kaplan PW, Ruegg S. Anesthetic drugs in status epilepticus: risk or rescue? A 6-year cohort study. Neurology. 2014;82:656–64.
Holtkamp M. Should barbiturates be used in refractory status epilepticus? J Clin Neurophysiol. 2016;33:22–4.
Zelano J, Kumlien E. Levetiracetam as alternative stage two antiepileptic drug in status epilepticus: a systematic review. Seizure. 2012;21:233–6.
Ramsay RE, Wilder BJ, Uthman BM, Garnett WR, Pellock JM, Barkley GL, Leppik IE, Knapp LE. Intramuscular fosphenytoin (Cerebyx) in patients requiring a loading dose of phenytoin. Epilepsy Res. 1997;28:181–7.
Wilder BJ, Campbell K, Ramsay RE, Garnett WR, Pellock JM, Henkin SA, Kugler AR. Safety and tolerance of multiple doses of intramuscular fosphenytoin substituted for oral phenytoin in epilepsy or neurosurgery. Arch Neurol. 1996;53:764–8.
Moreno Morales EY, Fernandez PM, Bondy Pena EC, Dominguez Lorenzo JM, Pardellas SE, Fernandez A. Observational study of intravenous lacosamide in patients with convulsive versus non-convulsive status epilepticus. Clin Drug Investig. 2015;35:463–9.
Garces M, Villanueva V, Mauri JA, Suller A, Garcia C, Lopez Gonzalez FJ, Rodriguez Osorio X, Fernandez Pajarín G, Piera A, Guillamon E, Santafe C, Castillo A, Giner P, Torres N, Escalza I, Del Villar A, Garcia de Casasola MC, Bonet M, Noe E, Olmedilla N. Factors influencing response to intravenous lacosamide in emergency situations: LACO-IV study. Epilepsy Behav. 2014;36:144–52.
Claassen J, Taccone FS, Horn P, Holtkamp M, Stocchetti N, Oddo M. Recommendations on the use of EEG monitoring in critically ill patients: consensus statement from the neurointensive care section of the ESICM. Intensive Care Med. 2013;39:1337–51.
Claassen J, Hirsch LJ, Emerson RG, Mayer SA. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43:146–53.
Rossetti AO, Milligan TA, Vulliemoz S, Michaelides C, Bertschi M, Lee JW. A randomized trial for the treatment of refractory status epilepticus. Neurocrit Care. 2011;14:4–10.
Claassen J, Hirsch LJ, Emerson RG, Bates JE, Thompson TB, Mayer SA. Continuous EEG monitoring and midazolam infusion for refractory nonconvulsive status epilepticus. Neurology. 2001;57:1036–42.
Fernandez A, Lantigua H, Lesch C, Shao B, Foreman B, Schmidt JM, Hirsch LJ, Mayer SA, Claassen J. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2014;82:359–65.
Bellante F, Legros B, Depondt C, Creteur J, Taccone FS, Gaspard N. Midazolam and thiopental for the treatment of refractory status epilepticus: a retrospective comparison of efficacy and safety. J Neurol. 2016;263:799–806.
Ulvi H, Yoldas T, Mungen B, Yigiter R. Continuous infusion of midazolam in the treatment of refractory generalized convulsive status epilepticus. Neurol Sci. 2002;23:177–82.
Parviainen I, Uusaro A, Kalviainen R, Mervaala E, Ruokonen E. Propofol in the treatment of refractory status epilepticus. Intensive Care Med. 2006;32:1075–9.
Cremer OL, Moons KG, Bouman EA, Kruijswijk JE, de Smet AM, Kalkman CJ. Long-term propofol infusion and cardiac failure in adult head-injured patients. Lancet. 2001;357:117–8.
Krajcova A, Waldauf P, Andel M, Duska F. Propofol infusion syndrome: a structured review of experimental studies and 153 published case reports. Crit Care. 2015;19:398.
Vasile B, Rasulo F, Candiani A, Latronico N. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med. 2003;29:1417–25.
Mirrakhimov AE, Voore P, Halytskyy O, Khan M, Ali AM. Propofol infusion syndrome in adults: a clinical update. Crit Care Res Pract. 2015;2015:260385.
Parviainen I, Uusaro A, Kalviainen R, Kaukanen E, Mervaala E, Ruokonen E. High-dose thiopental in the treatment of refractory status epilepticus in intensive care unit. Neurology. 2002;59:1249–51.
Prabhakar H, Kalaivani M. Propofol versus thiopental sodium for the treatment of refractory status epilepticus. Cochrane Database Syst Rev. 2017;2:CD009202.
Ferlisi M, Hocker S, Grade M, Trinka E, Shorvon S. Preliminary results of the global audit of treatment of refractory status epilepticus. Epilepsy Behav. 2015;49:318–24.
Byun JI, Chu K, Sunwoo JS, Moon J, Kim TJ, Lim JA, Jun JS, Lee HS, Lee WJ, Lee DY, Jeon D, Lee ST, Jung KH, Jung KY, Lee SK. Mega-dose phenobarbital therapy for super-refractory status epilepticus. Epileptic Disord. 2015;17:444–52.
Gaspard N, Foreman B, Judd LM, Brenton JN, Nathan BR, McCoy BM, Al-Otaibi A, Kilbride R, Fernandez IS, Mendoza L, Samuel S, Zakaria A, Kalamangalam GP, Legros B, Szaflarski JP, Loddenkemper T, Hahn CD, Goodkin HP, Claassen J, Hirsch LJ. Laroche Sm. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia. 2013;54:1498–503.
Höfler J, Rohracher A, Kalss G, Zimmermann G, Dobesberger J, Pilz G, Leitinger M, Kuchukhidze G, Butz K, Taylor A, Novak H, Trinka E. (S)-Ketamine in refractory and super-refractory status epilepticus: a retrospective study. CNS Drugs. 2016;30:869–76.
Sabharwal V, Ramsay E, Martinez R, Shumate R, Khan F, Dave H, Iwuchukwu I, McGrade H. Propofol-ketamine combination therapy for effective control of super-refractory status epilepticus. Epilepsy Behav. 2015;52:264–6.
Hijazi Y, Bodonian C, Bolon M, Salord F, Boulieu R. Pharmacokinetics and haemodynamics of ketamine in intensive care patients with brain or spinal cord injury. Br J Anaesth. 2003;90:155–60.
Mirsattari SM, Sharpe MD, Young GB. Treatment of refractory status epilepticus with inhalational anesthetic agents isoflurane and desflurane. Arch Neurol. 2004;61:1254–9.
Kofke WA, Young RS, Davis P, Woelfel SK, Gray L, Johnson D, Gelb A, Meeke R, Warner DS, Pearson KS. Isoflurane for refractory status epilepticus: a clinical series. Anesthesiology. 1989;71:653–9.
Zeiler FA, Zeiler KJ, Teitelbaum J, Gillman LM, West M. Modern inhalational anesthetics for refractory status epilepticus. Can J Neurol Sci. 2015;42:106–15.
Hanada T, Ido K, Kosasa T. Effect of perampanel, a novel AMPA antagonist, on benzodiazepine-resistant status epilepticus in a lithium-pilocarpine rat model. Pharmacol Res Perspect. 2014;2:e00063.
Rohracher A, Hofler J, Kalss G, Leitinger M, Kuchukhidze G, Deak I, Dobesberger J, Novak H, Pilz G, Zerbs A, Trinka E. Perampanel in patients with refractory and super-refractory status epilepticus in a neurological intensive care unit. Epilepsy Behav. 2015;49:354–8.
Redecker J, Wittstock M, Benecke R, Rosche J. Efficacy of perampanel in refractory nonconvulsive status epilepticus and simple partial status epilepticus. Epilepsy Behav. 2015;45:176–9.
Brigo F, Bragazzi NL, Igwe SC, Nardone R, Trinka E. Topiramate in the treatment of generalized convulsive status epilepticus in adults: a systematic review with individual patient data analysis. Drugs. 2017;77:67–74.
Kellinghaus C, Berning S, Stogbauer F. Use of oxcarbazepine for treatment of refractory status epilepticus. Seizure. 2014;23:151–4.
Novy J, Rossetti AO. Oral pregabalin as an add-on treatment for status epilepticus. Epilepsia. 2010;51:2207–10.
Walton NY, Jaing Q, Hyun B, Treiman DM. Lamotrigine vs. phenytoin for treatment of status epilepticus: comparison in an experimental model. Epilepsy Res. 1996;24:19–28.
Pruss H, Dalmau J, Harms L, Holtje M, Ahnert-Hilger G, Borowski K, Stoecker W, Wandinger KP. Retrospective analysis of NMDA receptor antibodies in encephalitis of unknown origin. Neurology. 2010;75:1735–9.
Holzer FJ, Rossetti AO, Heritier-Barras AC, Zumsteg D, Roebling R, Huber R, Lerche H, Kiphuth IC, Bardutzky J, Bien CG, Troger M, Schoch G, Pruss H, Seeck M. Antibody-mediated status epilepticus: a retrospective multicenter survey. Eur Neurol. 2012;68:310–7.
Gaspard N, Foreman BP, Alvarez V, Cabrera KC, Probasco JC, Jongeling AC, Meyers E, Espinera A, Haas KF, Schmitt SE, Gerard EE, Gofton T, Kaplan PW, Lee JW, Legros B, Szaflarski JP, Westover BM, Laroche SM, Hirsch LJ. New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology. 2015;85:1604–13.
Newman MP, Blum S, Wong RC, Scott JG, Prain K, Wilson RJ, Gillis D. Autoimmune encephalitis. Intern Med J. 2016;46:148–57.
Tollner K, Brandt C, Erker T, Loscher W. Bumetanide is not capable of terminating status epilepticus but enhances phenobarbital efficacy in different rat models. Eur J Pharmacol. 2015;746:78–88.
Pressler RM, Boylan GB, Marlow N, Blennow M, Chiron C, Cross JH, de Vries LS, Hallberg B, Hellstrom-Westas L, Jullien V, Livingstone V, Mangum B, Murphy B, Murray D, Pons G, Rennie J, Swarte R, Toet MC, Vanhatalo S, Zohar S. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): an open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 2015;14:469–77.
Reddy DS. Pharmacology of endogenous neuroactive steroids. Crit Rev Neurobiol. 2003;15:197–234.
Greenfield LJ Jr. Molecular mechanisms of antiseizure drug activity at GABAA receptors. Seizure. 2013;22:589–600.
Rosenthal ES, Claassen J, Wainwright MS, Husain AM, Vaitkevicius H, Raines S, Hoffmann E, Colquhoun H, Doherty JJ, Kanes SJ. Brexanolone as adjunctive therapy in super-refractory status epilepticus. Ann Neurol. 2017;82:342–52.
http://investor.sagerx.com/news-releases/news-release-details/sage-therapeutics-reports-top-line-results-phase-3-status-trial. Last access 16 Dec 2017.
Rho JM. How does the ketogenic diet induce anti-seizure effects? Neurosci Lett. 2017;637:4–10.
Sada N, Lee S, Katsu T, Otsuki T, Inoue T. Epilepsy treatment. Targeting LDH enzymes with a stiripentol analog to treat epilepsy. Science. 2015;347:1362–7.
Peterman MG. The ketogenic diet in epilepsy. JAMA. 1925;84:1979–83.
Gama IR, Trindade-Filho EM, Oliveira SL, Bueno NB, Melo IT, Cabral-Junior CR, Barros EM, Galvao JA, Pereira WS, Ferreira RC, Domingos BR, da Rocha AT. Effects of ketogenic diets on the occurrence of pilocarpine-induced status epilepticus of rats. Metab Brain Dis. 2015;30:93–8.
Thakur KT, Probasco JC, Hocker SE, Roehl K, Henry B, Kossoff EH, Kaplan PW, Geocadin RG, Hartman AL, Venkatesan A, Cervenka MC. Ketogenic diet for adults in super-refractory status epilepticus. Neurology. 2014;82:665–70.
Cervenka MC, Hocker S, Koenig M, Bar B, Henry-Barron B, Kossoff EH, Hartman AL, Probasco JC, Benavides DR, Venkatesan A, Hagen EC, Dittrich D, Stern T, Radzik B, Depew M, Caserta FM, Nyquist P, Kaplan PW, Geocadin RG. Phase I/II multicenter ketogenic diet study for adult superrefractory status epilepticus. Neurology. 2017;88:938–43.
Volgushev M, Kudryashov I, Chistiakova M, Mukovski M, Niesmann J, Eysel UT. Probability of transmitter release at neocortical synapses at different temperatures. J Neurophysiol. 2004;92:212–20.
Yang XF, Ouyang Y, Kennedy BR, Rothman SM. Cooling blocks rat hippocampal neurotransmission by a presynaptic mechanism: observations using 2-photon microscopy. J Physiol. 2005;567:215–24.
Schiff SJ, Somjen GG. The effects of temperature on synaptic transmission in hippocampal tissue slices. Brain Res. 1985;345:279–84.
Aihara H, Okada Y, Tamaki N. The effects of cooling and rewarming on the neuronal activity of pyramidal neurons in guinea pig hippocampal slices. Brain Res. 2001;893:36–45.
Liu Z, Gatt A, Mikati M, Holmes GL. Effect of temperature on kainic acid-induced seizures. Brain Res. 1993;631:51–8.
Schmitt FC, Buchheim K, Meierkord H, Holtkamp M. Anticonvulsant properties of hypothermia in experimental status epilepticus. Neurobiol Dis. 2006;23:689–96.
Kowski AB, Kanaan H, Schmitt FC, Holtkamp M. Deep hypothermia terminates status epilepticus–an experimental study. Brain Res. 2012;1446:119–26.
Zeiler FA, Zeiler KJ, Teitelbaum J, Gillman LM, West M. therapeutic hypothermia for refractory status epilepticus. Can J Neurol Sci. 2015;42:221–9.
Legriel S, Lemiale V, Schenck M, Chelly J, Laurent V, Daviaud F, Srairi M, Hamdi A, Geri G, Rossignol T, Hilly-Ginoux J, Boisrame-Helms J, Louart B, Malissin I, Mongardon N, Planquette B, Thirion M, Merceron S, Canet E, Pico F, Tran-Dinh YR, Bedos JP, Azoulay E, Resche-Rigon M, Cariou A. Hypothermia for neuroprotection in convulsive status epilepticus. N Engl J Med. 2016;375:2457–67.
Basha MM, Suchdev K, Dhakar M, Kupsky WJ, Mittal S, Shah AK. Acute resective surgery for the treatment of refractory status epilepticus. Neurocrit Care. 2017;27:370–80.
Acknowledgements
MH holds the “Friedrich-von-Bodelschwingh Endowed Professorship for Clinical and Experimental Epileptology” at the Department of Neurology at the Charité – Universitätsmedizin Berlin funded by von Bodelschwingh Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
Martin Holtkamp received speaker’s honoraria and/or consultancy fees within the last 5 years from Bial, Desitin, Eisai, LivaNova, Novartis, Shire, and UCB.
Rights and permissions
About this article
Cite this article
Holtkamp, M. Pharmacotherapy for Refractory and Super-Refractory Status Epilepticus in Adults. Drugs 78, 307–326 (2018). https://doi.org/10.1007/s40265-017-0859-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0859-1