Abstract
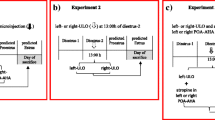
Hormonal and neural signals regulate the ovarian follicular development. The present study’s hypothesis is that the blockade of ovarian dopamine receptors locally will affect follicle development and ovulation. Groups of adult 4-day cyclic rats of the CII-ZV strain on estrus, diestrus-1, diestrus-2, or proestrus day were injected with vehicle, haloperidol (DA2 > DA1 blocker), sulpiride (DA2 blocker), or SCH-23390 (DA1 blocker) into the bursa of both ovaries at 08:00, 13:00, or 20:00 h. Animals were sacrificed the following predicted estrus day. The following treatments blocked ovulation: injecting haloperidol to rats on estrus or diestrus-1 at 8:00, 13:00, or 20:00 h and to rats on diestrus-2 at 08:00, or 20:00 h; injecting SCH-23390 to rats on diestrus-1 at 8:00, 13:00, or 20:00 h; injecting sulpiride to rats on estrus at 20:00 h, diestrus-1 at 08:00, 13:00, or 20:00 h and to rats on diestrus-2 at 08:00 h. In rats treated with any of the dopamine antagonists that blocked ovulation, injecting GnRH at 14.00 h on the next predicted proestrus day restored ovulation. Injecting estradiol benzoate at 14.00 h of the next predicted diestrus-2 restored ovulation in some animals treated with haloperidol on estrus or diestrus-2 and was ineffective in rats treated on diestrus-1. In rats treated with sulpiride or SCH-23390 ovulation occurred in most animals (SCH-23390: 6/8; SPD: 9/12). Present results suggest that dopamine ovarian receptors’ participation in regulating follicular development and ovulation varies along the estrus cycle, with their most prominent activity occurring on diestrus-1.







Similar content being viewed by others
References
L.I. Aguado, Role of the central and peripheral nervous system in the ovarian function. Microsc. Res. Tech. 59(6), 462–473 (2002). doi:10.1002/jemt.10232
I. Gerendai, P. Banczerowski, B. Halasz, Functional significance of the innervation of the gonads. Endocrine 28(3), 309–318 (2005). doi:10.1385/ENDO:28:3:309
A. Mayerhofer, H.C. Hemmings Jr, G.L. Snyder, P. Greengard, S. Boddien, U. Berg, C. Brucker, Functional dopamine-1 receptors and DARPP-32 are expressed in human ovary and granulosa luteal cells in vitro. J. Clin. Endocrinol. Metab. 84(1), 257–264 (1999). doi:10.1210/jcem.84.1.5378
A. Mayerhofer, G.D. Smith, M. Danilchik, J.E. Levine, D.P. Wolf, G.A. Dissen, S.R. Ojeda, Oocytes are a source of catecholamines in the primate ovary: evidence for a cell-cell regulatory loop. Proc. Natl. Acad. Sci. USA 95(18), 10990–10995 (1998)
H. D’Albora, J.J. Barcia, Intrinsic neuronal cell bodies in the rat ovary. Neurosci. Lett. 205(1), 65–67 (1996)
W.L. Dees, J.K. Hiney, T.D. Schultea, A. Mayerhofer, M. Danilchik, G.A. Dissen, S.R. Ojeda, The primate ovary contains a population of catecholaminergic neuron-like cells expressing nerve growth factor receptors. Endocrinology 136(12), 5760–5768 (1995). doi:10.1210/endo.136.12.7588334
H. D’Albora, P. Lombide, S.R. Ojeda, Intrinsic neurons in the rat ovary: an immunohistochemical study. Cell Tissue Res. 300(1), 47–56 (2000)
P.G. Hofmann, A. Baez Saldana, T. Fortoul Van Der Goes, M. Gonzalez del Pliego, G. Gutierrez Ospina, Neuroendocrine cells are present in the domestic fowl ovary. J. Anat. 222(2), 170–177 (2013). doi:10.1111/joa.12002
J.M. Bahr, N. Ben-Jonathan, Preovulatory depletion of ovarian catecholamines in the rat. Endocrinology 108(5), 1815–1820 (1981). doi:10.1210/endo-108-5-1815
P.A. Denning-Kendall, M.L. Wild, D.C. Wathes, Regional differences in catecholamine concentrations in bovine ovaries analysed by high-performance liquid chromatography. J. Endocrinol. 129(2), 221–226 (1991)
A. Mayerhofer, S. Fritz, R. Grunert, S.L. Sanders, D.M. Duffy, S.R. Ojeda, R.L. Stouffer, D1-Receptor, DARPP-32, and PP-1 in the primate corpus luteum and luteinized granulosa cells: evidence for phosphorylation of DARPP-32 by dopamine and human chorionic gonadotropin. J. Clin. Endocrinol. Metab. 85(12), 4750–4757 (2000). doi:10.1210/jcem.85.12.7084
S.S. King, A.G. Campbell, E.A. Dille, J.F. Roser, L.L. Murphy, K.L. Jones, Dopamine receptors in equine ovarian tissues. Domest. Anim. Endocrinol. 28(4), 405–415 (2005). doi:10.1016/j.domaniend.2005.02.001
S.S. King, K.L. Jones, B.A. Mullenix, D.T. Heath, Seasonal relationships between dopamine D1 and D2 receptor and equine FSH receptor mRNA in equine ovarian epithelium. Anim. Reprod. Sci. 108(1–2), 259–266 (2008). doi:10.1016/j.anireprosci.2007.08.007
V. Rey-Ares, N. Lazarov, D. Berg, U. Berg, L. Kunz, A. Mayerhofer, Dopamine receptor repertoire of human granulosa cells. Reprod. Biol. Endocrinol. 5, 40 (2007). doi:10.1186/1477-7827-5-40
R. Dominguez, C.M. Gaitan, S.A. Mendez, A. Ulloa-Aguirre, Effects of catecholaminergic blockade by haloperidol or propranolol at different stages of the oestrous cycle on ovulation and gonadotrophin levels in the rat. J. Endocrinol. 113(1), 37–44 (1987)
R. Dominguez, D. Zipitría, L. Riboni, R. Revilla, Differences in the ability of reserpine and chlorpromazine to block ovulation throughout the estrous cycle of the rat. J. Interdiscip. Cycle Res. 16(1), 63–72 (1985). doi:10.1080/09291018509359872
S. Isobe, The role of the dopaminergic system in the rat ovary. Nihon Naibunpi Gakkai Zasshi 70(4), 457–464 (1994)
H. Mori, S. Arakawa, T. Ohkawa, R. Ohkawa, S. Takada, T. Morita, S. Okinaga, The involvement of dopamine in the regulation of steroidogenesis in rat ovarian cells. Horm. Res. 41(Suppl 1), 36–40 (1994)
J. Bodis, M. Koppan, L. Kornya, H.R. Tinneberg, A. Torok, The effect of catecholamines, acetylcholine and histamine on progesterone release by human granulosa cells in a granulosa cell superfusion system. Gynecol. Endocrinol. 16(4), 259–264 (2002)
F. Papenfuss, J. Bodis, H.R. Tinneberg, H. Schwarz, The modulatory effect of catecholamines on gonadotropin-stimulated granulosa cell steroid secretion. Arch. Gynecol. Obstet. 253(2), 97–102 (1993)
M.L. Rankin, L.A. Hazelwood, R. Benjamin Freer, Y. Namkung, B.E. Rex, R.A. Roof, D.R. Sibley, Molecular pharmacology of the dopamine receptors, in Dopamine handbook, vol. 1, ed. by L.L. Iversen, D.S. Iversen, S.B. Dunnett, A. Bjorklund (Oxford University Press, New York, 2010), pp. 63–87
G. Emilien, J.M. Maloteaux, M. Geurts, K. Hoogenberg, S. Cragg, Dopamine receptors: physiological understanding to therapeutic intervention potential. Pharmacol. Ther. 84(2), 133–156 (1999)
C. Moran, A. Franco, J.L. Moran, A. Handal, L. Morales, R. Dominguez, Neural activity between ovaries and the prevertebral celiac-superior mesenteric ganglia varies during the estrous cycle of the rat. Endocrine 26(2), 147–152 (2005). doi:10.1385/endo:26:2:147
C. Moran, F. Zarate, J.L. Moran, A. Handal, R. Dominguez, Lateralization of the connections of the ovary to the celiac ganglia in juvenile rats. Reprod. Biol. Endocrinol. 7, 50 (2009). doi:10.1186/1477-7827-7-50
G. Rosas, M.I. Ramirez, R. Linares, A. Trujillo, R. Dominguez, L. Morales-Ledesma, Asymmetric steroidogenic response by the ovaries to the vasoactive intestinal peptide. Endocrine 48(3), 968–977 (2015). doi:10.1007/s12020-014-0449-x
J.L. Moran, M.E. Cruz, R. Dominquez, Differences in the ovulatory response to unilateral lesions in the preoptic or anterior hypothalamic area performed on each day of the estrous cycle of adult rats. Brain Res. Bull. 33(6), 663–668 (1994)
J.L. Moran, R. Dominguez, Effects of the unilateral implant of haloperidol at the preoptic-anterior hypothalamic area, on ovulation. Endocrine 3(6), 391–393 (1995). doi:10.1007/bf02935642
R.F. Weick, E.R. Smith, R. Dominguez, A.P. Dhariwal, J.M. Davidson, Mechanism of stimulatory feedback effect of estradiol benzoate on the pituitary. Endocrinology 88(2), 293–301 (1971). doi:10.1210/endo-88-2-293
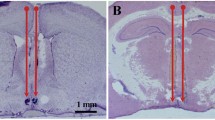
A. Díaz, L. De Jesús, L. Mendieta, M. Calvillo, B. Espinosa, E. Zenteno, J. Guevara, I.D. Limón, The amyloid-β25–35 injection into the CA1 region of the neonatal rat hippocampus impairs the long-term memory because of an increase of nitric oxide. Neurosci. Lett. 468(2), 151–155 (2010). doi:10.1016/j.neulet.2009.10.087
C.A. Schneider, W.S. Rasband, K.W. Eliceiri, NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 9(7), 671–675 (2012)
F.X. Donadeu, O.J. Ginther, Follicular waves and circulating concentrations of gonadotrophins, inhibin and oestradiol during the anovulatory season in mares. Reprod. (Camb. Engl.) 124(6), 875–885 (2002)
G. Mari, M. Morganti, B. Merlo, C. Castagnetti, F. Parmeggiani, N. Govoni, G. Galeati, C. Tamanini, Administration of sulpiride or domperidone for advancing the first ovulation in deep anestrous mares. Theriogenology 71(6), 959–965 (2009). doi:10.1016/j.theriogenology.2008.11.001
L. Zoldag, S. Fekete, I. Csaky, A. Bersenyi, Fertile estrus induced in bitches by bromocryptine, a dopamine agonist: a clinical trial. Theriogenology 55(8), 1657–1666 (2001)
M.J. Fell, J.C. Neill, K.M. Marshall, Effects of the classical antipsychotic haloperidol and atypical antipsychotic risperidone on weight gain, the oestrous cycle and uterine weight in female rats. Eur. Neuropsychopharmcol. 14(5), 385–392 (2004). doi:10.1016/j.euroneuro.2003.12.001
K. Maeda, S. Ohkura, Y. Uenoyama, Y. Wakabayashi, Y. Oka, H. Tsukamura, H. Okamura, Neurobiological mechanisms underlying GnRH pulse generation by the hypothalamus. Brain Res. 1364, 103–115 (2010). doi:10.1016/j.brainres.2010.10.026
N.P. Evans, G.E. Dahl, D.T. Mauger, V. Padmanabhan, L.A. Thrun, F.J. Karsch, Does estradiol induce the preovulatory gonadotropin-releasing hormone (GnRH) surge in the ewe by inducing a progressive change in the mode of operation of the GnRH neurosecretory system. Endocrinology 136(12), 5511–5519 (1995). doi:10.1210/endo.136.12.7588302
M.E. Freeman, Chapter 43: neuroendocrine control of the ovarian cycle of the rat, in Knobil and Neill’s physiology of reproduction, 3rd edn., ed. by J.D. Neill, T.M. Plant, D.W. Pfaff, J.R.G. Challis, DMd Kretser, J.S. Richards, P.M. Wassarman (Academic Press, St Louis, 2006), pp. 2327–2388
N.P. Evans, G.E. Dahl, V. Padmanabhan, L.A. Thrun, F.J. Karsch, Estradiol requirements for induction and maintenance of the gonadotropin-releasing hormone surge: implications for neuroendocrine processing of the estradiol signal. Endocrinology 138(12), 5408–5414 (1997). doi:10.1210/endo.138.12.5558
J.W. Everett, Central neural control of reproductive functions of the adenohypophysis. Physiol. Rev. 44(3), 373–431 (1964)
T. Baptista, E. Araujo de Baptista, N.M. Ying Kin, S. Beaulieu, D. Walker, R. Joober, J. Lalonde, D. Richard, Comparative effects of the antipsychotics sulpiride or risperidone in rats I: bodyweight, food intake, body composition, hormones and glucose tolerance. Brain Res. 957(1), 144–151 (2002)
B.J. Kinon, J.A. Gilmore, H. Liu, U.M. Halbreich, Hyperprolactinemia in response to antipsychotic drugs: characterization across comparative clinical trials. Psychoneuroendocrinology 28(Suppl 2), 69–82 (2003)
M. Goiny, S. Cekan, K. Uvnas-Moberg, Effects of dopaminergic drugs on plasma levels of steroid hormones in conscious dogs. Life Sci. 38(25), 2293–2300 (1986)
L.A. Arbogast, N. Ben-Jonathan, The preovulatory prolactin surge is prolonged by a progesterone-dependent dopaminergic mechanism. Endocrinology 126(1), 246–252 (1990). doi:10.1210/endo-126-1-246
Y. Taketa, M. Yoshida, K. Inoue, M. Takahashi, Y. Sakamoto, G. Watanabe, K. Taya, J. Yamate, A. Nishikawa, Differential stimulation pathways of progesterone secretion from newly formed corpora lutea in rats treated with ethylene glycol monomethyl ether, sulpiride, or atrazine. Toxicol. Sci. 121(2), 267–278 (2011). doi:10.1093/toxsci/kfr062
S. Mostafapour, S. Zare, R.A. Sadrkhanlou, A. Ahmadi, M. Razi, Sulpiride-induced hyperprolactinemia in mature female rats: evidence for alterations in the reproductive system, pituitary and ovarian hormones. Int. J. Fertil. Steril. 8(2), 193–206 (2014)
G. Macchiarelli, S.A. Nottola, M.G. Palmerini, S. Bianchi, M. Maione, C. Lorenzo, G. Stifano, E. Di Marco, S. Correr, Morphological expression of angiogenesis in the mammalian ovary as seen by SEM of corrosion casts. Italian J. Anat. Embryol. 115(1–2), 109–114 (2010)
F. Delgado-Rosas, R. Gomez, H. Ferrero, F. Gaytan, J. Garcia-Velasco, C. Simon, A. Pellicer, The effects of ergot and non-ergot-derived dopamine agonists in an experimental mouse model of endometriosis. Reprod. (Camb. Engl.) 142(5), 745–755 (2011). doi:10.1530/rep-11-0223
R. Gomez, H. Ferrero, F. Delgado-Rosas, M. Gaytan, C. Morales, R.C. Zimmermann, C. Simon, F. Gaytan, A. Pellicer, Evidences for the existence of a low dopaminergic tone in polycystic ovarian syndrome: implications for OHSS development and treatment. J. Clin. Endocrinol. Metab. 96(8), 2484–2492 (2011). doi:10.1210/jc.2011-0075
R. Gomez, M. Gonzalez-Izquierdo, R.C. Zimmermann, E. Novella-Maestre, I. Alonso-Muriel, J. Sanchez-Criado, J. Remohi, C. Simon, A. Pellicer, Low-dose dopamine agonist administration blocks vascular endothelial growth factor (VEGF)-mediated vascular hyperpermeability without altering VEGF receptor 2-dependent luteal angiogenesis in a rat ovarian hyperstimulation model. Endocrinology 147(11), 5400–5411 (2006). doi:10.1210/en.2006-0657
C.C. Ouimet, P.E. Miller, H.C. Hemmings Jr, S.I. Walaas, P. Greengard, DARPP-32, a dopamine- and adenosine 3′:5′-monophosphate-regulated phosphoprotein enriched in dopamine-innervated brain regions. III. Immunocytochemical localization. J. Neurosci. 4(1), 111–124 (1984)
Acknowledgments
This work was supported by CONACYT Grant 316181 to B. Venegas. We thank MSc Alvaro Domínguez-González for the assistance in the English revision.
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Venegas-Meneses, B., Padilla, J.F., Juárez, C.E. et al. Effects of ovarian dopaminergic receptors on ovulation. Endocrine 50, 783–796 (2015). https://doi.org/10.1007/s12020-015-0636-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0636-4