Abstract
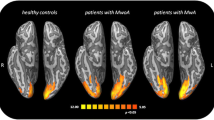
Chronic migraine is a relatively common disorder in neurological terms that causes very significant disability at a high cost. The precise mechanisms behind the progression of episodic migraine to chronic migraine are not well understood. Functional neuro-imaging works on the basis that neuronal activations are associated with changes in regional cerebral blood flow, and it can help us answer some of these questions. In this review, we discuss important recent studies in chronic migraine or studies relating to increasing frequency of migraine attacks. The findings show that increasing frequency of migraine attacks is associated with changes in key brainstem areas, basal ganglia and various cortical areas involved in pain.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Natoli JL, Manack A, Dean B, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30:599–609.
Headache disorders. Fact sheet N°277. http://www.who.int/mediacentre/factsheets/fs277/en/. Accessed Jan 2013.
Bloudek LM, Stokes M, Buse DC, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain. 2012;13:361–78.
Headache Classification Committee of The International Headache Society. International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004, 24: 1–160.
Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain. 2010;11:289–99.
Bigal ME, Serrano D, Buse D, et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. 2008;48:1157–68.
Manack A, Buse DC, Serrano D, Turkel CC, Lipton RB. Rates, predictors, and consequences of remission from chronic migraine to episodic migraine. Neurology. 2011;76:711–8.
Bigal ME, Lipton RB. Obesity is a risk factor for transformed migraine but not chronic tension-type headache. Neurology. 2006;67(2):252–7.
Ashina S, Serrano D, Lipton RB, et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13:615–24.
Katsarava Z, Schneeweiss S, Kurth T, et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology. 2004;62:788–90.
Frackowiak RSJ, Friston KJ. Functional neuroanatomy of the human brain: positron emission tomography—a new neuroanatomical technique. J Anat. 1994;184:211–25.
Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995;1:658–60.
Matharu MS, Bartsch T, Ward N, et al. Central neuromodulation in chronic migraine patients with suboccipital stimulators: a PET study. Brain. 2004;127(Pt 1):220–30.
Obermann M, Gizewski ER, Limmroth V, Diener HC, Katsarava Z. Symptomatic migraine and pontine vascular malformation: evidence for a key role of the brainstem in the pathophysiology of chronic migraine. Cephalalgia. 2006;26:763–6.
Goadsby PJ. Neurovascular headache and a midbrain vascular malformation: evidence for a role of the brainstem in chronic migraine. Cephalalgia. 2002;22:107–11.
• Grazzi L, Chiapparini L, Ferraro S, et al. Chronic migraine with medication overuse pre-post withdrawal of symptomatic medication: clinical results and FMRI correlations. Headache. 2010;50:998–1004. This study shows that MOH is associated with reversible changes in the lateral pain system involved in the localization, intensity and quality of pain.
Fumal A, Laureys S, Di Clemente L, et al. Orbitofrontal cortex involvement in chronic analgesic-overuse headache evolving from episodic migraine. Brain. 2006;129(Pt 2):543–50.
London ED, Cascella NG, Wong DF, et al. Cocaine-induced reduction of glucose utilization in human brain. A study using positron emission tomography and [fluorine 18]-fluorodeoxyglucose. Arch Gen Psychiatry. 1990;47:567–74.
Volkow ND, Fowler JS, Wolf AP, et al. Changes in brain glucose metabolism in cocaine dependence and withdrawal. Am J Psychiatry. 1991;148:621–6.
London ED, Ernst M, Grant S, Bonson K, Weinstein A. Orbitofrontal cortex and human drug abuse: functional imaging. Cereb Cortex. 2000;10:334–42.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain viewed in the light of imaging studies: brain circuits and treatment strategies. Neuropharmacology. 2004;47 Suppl 1:3–13.
Katsarava Z, Muessig M, Dzagnizde A, et al. Medication overuse headache: rates and predictors for relapse in a 4-year prospective study. Cephalalgia. 2004;25:12–5.
Fritsche G, Eberl A, Katsarava Z, Limmoroth V, Diener HC. Drug-induced headache: long-term follow up of withdrawal therapy and persistence of drug misuse. Eur Neurol. 2001;45:229–35.
Grazzi L, Andrasik F, D’Amico D, et al. Behavioral and pharmacologic treatment of transformed migraine with analgesic overuse: outcome at 3 years. Headache. 2002;59:1011–114.
• Maleki N, Becerra L, Brawn J, et al.: Common hippocampal structural and functional changes in migraine. Brain Struct Funct. 2012, Jul 4. doi: 10.1007/s00429‐012‐0437‐y. PMID: 22760159. This study associates hippocampal changes of reduced volume, greater activation in response to pain and reduced functional connectivity to pain-related cortical areas with increasing frequency of migraine attacks, probably relating to the involvement of the hippocampus in the stress response.
McEwen BS. Stress and hippocampal plasticity. Annu Rev Neurosci. 1999;22:105–22.
McEwen BS. Plasticity of the hippocampus: adaptation to chronic stress and allostatic load. Ann N Y Acad Sci. 2001;933:265–77.
McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222.
Rodrigues SM, LeDoux JE, Sapolsky RM. The influence of stress hormones on fear circuitry. Annu Rev Neurosci. 2009;32:289–313.
Cui Z, Gerfen CR, Young WS 3rd. Hypothalamic and other connections with the dorsal CA2 area of the mouse hippocampus. J Comp Neurol. 2012 Nov 21. doi: 10.1002/cne.23263. PMID:23172108
•• Maleki N, Becerra L, Nutile L, et al. Migraine attacks the Basal Ganglia. Mol Pain. 2011;7:71. This study associates the basal ganglia findings of increased volume and reduced activations in response to pain with increasing frequency of migraine attacks.
•• Starr CJ, Sawaki L, Wittenberg GF, et al. The contribution of the putamen to sensory aspects of pain: insights from structural connectivity and brain lesions. Brain. 2011;134(Pt 7):1987–2004. The findings of this study suggest that the putamen and the basal ganglia are involved in the sensory experience of pain beyond the well-known role in pain-related motor responses via the cortico-basal ganglia-thalamo-cortical loops.
Afridi SK, Matharu MS, Lee L, et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain. 2005;128(Pt 4):932–9.
May A, Bahra A, Büchel C, Frackowiak RS, Goadsby PJ. Hypothalamic activation in cluster headache attacks. Lancet. 1998;352:275–8.
Kruit MC, Launer LJ, Overbosch J, van Buchem MA, Ferrari MD. Iron accumulation in deep brain nuclei in migraine: a population-based magnetic resonance imaging study. Cephalalgia. 2009;29:351–9.
Tepper SJ, Lowe MJ, Beall E, etal.: Iron deposition in pain-regulatory nuclei in episodic migraine and chronic daily headache by MRI. 2012;52:236–43.
Hallgren B, Sourander P. The effect of age on the non-haemin iron in the human brain. J Neurochem. 1958;3:41–51.
Valfrè W, Rainero I, Bergui M, Pinessi L. Voxel-based morphometry reveals gray matter abnormalities in migraine. Headache. 2008;48:109–17.
Price DD. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–72.
Lai TH, Fuh JL, Lirng JF, Lin CP, Wang SJ. Brainstem 1H-MR spectroscopy in episodic and chronic migraine. J Headache Pain. 2012;13(8):645–51.
Kong J, Tu PC, Zyloney C, Su TP. Intrinsic functional connectivity of the periaqueductal gray, a resting fMRI study. Behav Brain Res. 2010;211:215–9.
• Mainero C, Boshyan J, Hadjikhani N. Altered functional magnetic resonance imaging resting-state connectivity in periaqueductal gray networks in migraine. Ann Neurol. 2011;70:838–45. This study shows reduced functional connectivity of the PAG with prefrontal cortex, ACC and amygdala correlating with increasing frequency of migraine attacks.
Knight YE, Goadsby PJ. The periaqueductal grey matter modulates trigeminovascular input: a role in migraine? Neuroscience. 2001;106:793–800.
Kato Y, Araki N, Matsuda H, Ito Y, Suzuki C. Arterial spin-labeled MRI study of migraine attacks treated with rizatriptan. J Headache Pain. 2010;11:255–8.
Conflict of Interest
Dr. Farooq Maniyar declares that he has no conflict of interest.
Dr. Peter J. Goadsby declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Chronic Daily Headache
Rights and permissions
About this article
Cite this article
Maniyar, F.H., Goadsby, P.J. Functional Imaging in Chronic Migraine. Curr Pain Headache Rep 17, 333 (2013). https://doi.org/10.1007/s11916-013-0333-z
Published:
DOI: https://doi.org/10.1007/s11916-013-0333-z