Abstract
Matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs) play a significant role in regulating angiogenesis, the process of new blood vessel formation. Interstitial collagenase (MMP-1), 72 kDa gelatinase A/type IV collagenase (MMP-2), and 92 kDa gelatinase B/type IV collagenase (MMP-9) dissolve ex- tracellular matrix (ECM) and may initiate and promote angiogenesis. TIMP-1, TIMP-2, TIMP-3, and possibly, TIMP-4 inhibit neovascularization. A new paradigm is emerging that matrilysin (MMP-7), MMP-9, and metal- loelastase (MMP-12) may block angiogenesis by converting plasminogen to angiostatin, which is one of the most potent angiogenesis antagonists. MMPs and TIMPs play a complex role in regulating angiogenesis. An understanding of the biochemical and cellular pathways and mechanisms of angiogenesis will provide important information to allow the control of angiogenesis, e.g. the stimulation of angiogenesis for coronary collateral circulation formation; while the inhibition for treating arthritis and cancer.
Similar content being viewed by others
Significance of matrix metalloproteinases in angiogenesis
Matrix metalloproteinases (MMPs) are a family of highly homologous zinc endopeptidases that cleave peptide bonds of the extracellular matrix (ECM) proteins, such as collagens, laminins, elastin, and fibronectin1, 2, 3. Both normal and transformed cells produce one or more members of the MMP family. This family of proteinases play a very important role in normal connective tissue turnover during morphogenesis, development, wound healing, reproduction, and neovascularization. Their proteolytic activities are controlled by a family of proteins called tissue inhibitors of metalloproteinases (TIMPs). The imbalance of the MMPs and TIMPs are implicated in many pathological processes such as the cancer metastasis, arthritis, inflammation, periodontal diseases, corneal ulceration, and cardiovascular diseases.
The process of new capillary blood vessel formation from preexisting blood vessels is called angiogenesis or neovascularization4. At the initial stage of new blood vessel formation, basement membrane, the specialized type IV collagen and lamininrich connective tissue membrane underlying endothelial cell layers, and interstitial connective tissue matrix, the type I and III collagen-rich ground substances, and type II collagen in cartilage, are broken down, therefore, angiogenesis requires digestion of the ECM barrier underlying the blood vessel endothelial cell layers by MMPs. New blood vessel formation plays a paramount role in normal development, reproduction, and wound healing. Wound healing, menstruation, embryo implantation and placentation, and embryo growth and morphogenesis all require new blood vessel formation to supply oxygen and nutrients. Coronary heart disease is the major cause of cardiovascular death. The blockage of a main coronary artery prevents the blood supply to the myocardium and leads to heart failure. Neovascularization is essential for providing oxygen and nutrients to the heart of a patient with coronary artery disease; the newly formed collateral circulation will allow blood flow to bypass the blocked coronary artery and supply blood to the heart to prevent heart attack. Angiogenic factors are attractive drug leads for stimulating collateral circulation formation in patients with coronary heart disease.
Neovascularization also plays a role in cancer growth and metastasis, inflammation, and rheumatoid arthritis. Uncontrolled and persistent angiogenesis is a cause of many diseases4. For example, hemangiomas and Kaposi's sarcoma are vascular tumors. Hemangiomas are composed of closely packed capillaries or abnormally dilated blood vessels and are characterized by the presence of endothelial and inflammatory cells; in diabetes, new capillaries in retina invade the vitreous, bleed, and cause blindness; ocular new blood vessel formation is the most common causes of blindness and dominates approximately twenty eye diseases. In arthritis, new capillary blood vessels invade to the joint and destroy cartilage structure. In addition, angiogenesis is critical for providing oxygen and nutrients for solid tumor growth and for generating a gateway for cancer cell spread to other parts of the body, such as lungs, liver, brain, or bones, through blood circulation system. Angiogenesis inhibitors may become one the most promising types of drugs for starving tumor cells and preventing the cancer cell growth and metastasis.
Collagen- degrading matrix metalloproteinases in angiogenesis
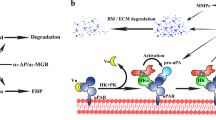
Neovascularization consists of a sequence of events that include dissolution of the basement membrane underlying the endothelial layer, migration and proliferation of endothelial cells, formation of the vascular capillary, and formation of a new basement membrane. Type IV collagenase activity is important in the early steps of endothelial morphogenesis, that is the migration of endothelial cells out of the existing blood vessels. Interstitial collagenase activity is responsible for the endothelial cell migration through the stromal interstitial spaces. The collagen-degrading enzymes are members of the MMP family1,2,3. Although individual members of the MMP family are different in their molecular mass (20-100 kDa) and protein substrate specificities, there is considerable gene and protein sequence homology and some overlap with their substrate specificities. Many of the MMPs are produced in soluble forms and some are transmembrane proteins. Types I, II, and III collagens can be digested effectively by fibroblast type collagenase (MMP-1), neutrophil type collagenase (MMP-8), and membrane type 1 matrix metalloproteinase (MT1-MMP, MMP-14). In addition, 72 kDa gelatinase A/type IV collagenase (MMP-2) can cleave both type I and type IV collagen effectively. The 92 kDa gelatinase B/type IV collagenase (MMP-9) has high catalytic activity towards type IV collagen. Furthermore, stromelysins also have some catalytic activity in hydrolyzing type IV collagen.
Capillary sprout formation is initiated by fragmentation of the capillary basal lamina and subsequent migration and proliferation of distinct endothelial cell populations in response to angiogenic stimuli4. Capillary blood vessels consist of endothelial cells and pericytes. These two cell types carry all the genetic information to form tubes, branches, and whole capillary networks. Specific angiogenic molecules can initiate this process whereas specific inhibitory molecules can stop it. Angiogenesis requires breakdown of the ECM by proteinases. The basement membrane, the specialized type IV collagen and laminin-rich membrane underlying blood vessel endothelial layers, the interstitial matrix that are the types I and III collagen-rich ground substance, and the type II collagen in cartilage, are fragmented during the process of new blood vessel formation.
Collagens are the matrix proteins best associated with angiogenesis in vivo, the loss of collagens leads to irreversible breakdown of matrix, identifying the collagenases as key enzymes in the initial steps of neovascularization5,6,7. To form a branch, the continuous basement membrane must be dissolved by proteinases first. The fragmentation of basement membrane type IV collagen is carried out by MMP-2 and MMP-95, 8. Type IV collagenase activity is important in the early steps of endothelial cell morphogenesis/capillary formation8. Interstitial collagenase (MMP-1) is also required for angiogenesis in vitro6. Vascular endothelial growth factor (VEGF) induces MMP-1 expression in human endothelial cells and MMP-1 is responsible for the initiation of degradation of interstitial collagen types I-III under normal physiological conditions9. MT1-MMP can also break down collagen types I-III, gelatin, laminin, and other ECM components in addition to activating pro-MMP-21,2,3. MT1-MMP is expressed by endothelial cells and it may regulate angiogenesis by activating pro-MMP2 and by cleaving collagens on the cell surface at a highly localized site10.
Tissue inhibitors of metalloproteinases in neovascularization
Tissue inhibitor of metalloproteinases (TIMP) family regulate ECM turnover and tissue remodeling by forming tight-binding inhibitory complexes with the MMPs11. Each member of the TIMP family can inhibit all the active MMPs with certain degree of preferences. TIMPs are multifunctional proteins that have erythroid-potentiating and cell-growth-promoting activities in addition to anti-MMP activities3, 12. A TIMP-like anti-angiogenic protein was identified from cartilage7. The TIMP family play an important role in angiogenesis through anti-MMP dependent and/or independent pathways5, 7.
Tissue inhibitor of metalloproteinases 1 (TIMP-1) is a 28.5 kDa glycoprotein. It blocks the endothelial cell response to angiogenic factors, e.g., basic fibroblast growth factor (bFGF), in an in vivo rat corneal angiogenesis assay13. The TIMP-1 effect is mediated in part through the inhibition of endothelial cell migration, as determined by the ability of TIMP 1 to block chemotaxis in a Boyden chamber assay. However, the angiogenesis inhibitory activity of TIMP-1 may not be related to its anti-metalloproteinase activity; TIMP-1 may affect cellular function in different ways. A 29 kDa recombinant TIMP-1 inhibits MMP activity, but a 66 kDa aggregate of TIMP-1 does not block MMP activity. Interestingly, both the 29 kDa TIMP-1 and the 66 kDa TIMP-1 aggregate inhibit in vitro angiogenesis14.
Tissue inhibitor of metalloproteinases-2 (TIMP-2) has a molecular mass of 21 kDa and it does not have any N-glycosylation site. Both TIMP-1 and TIMP-2 decrease endothelial tube formation on the ECM Matrigel8. TIMP-2 is a potent MMP inhibitor that can bind to both latent and active form of MMP-2. TIMP-2 inhibits bFGF-induced human microvascular endothelial cell proliferation15. However, TIMP-1 does not slow the growth of these cells. Furthermore, neither BB94, a broad spectrum and potent synthetic MMP inhibitor, nor antibodies to MMP-2 inhibit endothelial cell proliferation under the conditions tested, suggesting that anti-MMP activity does not block endothelial cell growth15. Cell adhesion to tissue culture plastic is slightly stimulated by TIMP-2 and cell migration is inhibited with short-term exposure to TIMP-2, but neither process is affected by long-term exposure. The ability of TIMP-2 to slow the endothelial cell proliferation in culture unrelated to its metalloproteinase-inhibitory activity indicates that TIMP-2 may have unique functions that may restrict angiogenesis associated with tumor growth and metastasis.
Although other members of the TIMP family are present in soluble forms, tissue inhibitor of metalloproteinases-3 (TIMP-3) is insoluble and is bound to the ECM12, 16. TIMP-3 is a 21 kDa unglycosylated protein although it has one potential N-glycosylation site. TIMP-3 inhibits chemotaxis of vascular endothelial cells toward VEGF and bFGF, collagen gel invasion and capillary morphogenesis in vitro, and bFGF-induced angiogenesis in the chicken chorioallantoic membrane (CAM) assay in vivo16. Tissue inhibitor of metalloproteinase-4 (TIMP-4) has a molecular mass of 22.4 kDa and it does not have any N-glycosylation site. TIMP-4 expresses at the highest level in heart and it can inhibit breast cancer growth and metastasis in athymic nude mice presumably due to its anti-angiogenic activity11, 17. In summary, TIMPs are able to regulate endothelial cell proliferation, migration, and capillary tube formation.
New paradigm of role of MMPs in angiogenesis: plasminogen angiostatin converting enzyme activities
Although a body of evidence has demonstrated that MMPs promote and TIMPs block angiogenesis, it seems paradoxical that some members of the MMP family may act as angiogenesis antagonists. One of the most potent natural inhibitors of angiogenesis is angiostatin4, 18. Angiostatin is a 38 kDa protein fragment that is derived from the first four kringle domains of plasminogen molecule. Angiostatin, not intact plasminogen, is a novel and very potent angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. It is a specific inhibitor of endothelial cell proliferation and angiogenesis, and tumor growth and metastasis. Because angiogenesis inhibitors do not induce multidrug resistance, they may be a class of the most potent and promising drugs for clinical treatment of cancer and other types of connective tissue diseases. Thus, the identification of the plasminogen-angiostatin converting enzymes is of paramount clinical importance. A clarification of the molecular mechanisms of generating angiostatin is essential to an understanding of biochemical pathways of controlling angiogenesis.
Unexpected results have challenged the old paradigms that MMPs can stimulate angiogenesis and inhibitors of MMPs can block angiogenesis. Dr. Fidler and associates show that macrophage-derived metalloelastase (MMP-12) is responsible for the generation of angiostatin in Lewis lung carcinoma19. We have also demonstrated that matrilysin (MMP-7) and gelatinase B/type IV collagenase (MMP-9) hydrolyze human plasminogen to generate angiostatin fragments20. The cleavage sites have been determined. MMP-7 cleaves the Pro (466) -Val (467) peptide bond and MMP-9, the Pro (465) -Pro (466) bond, between kringle domain 4 and 5 of the plasminogen molecule. The physiological relevance and significance of the production of angiostatin by MMP-7 and MMP-9 in vivo remain to be investigated. We are in the process of investigating if any other members of the MMP family can also convert plasminogen to angiostatin molecules. The specificity, efficiency, detailed cleavage sites, biological activities, and physiological relevance of angiostatin fragments generated by different enzymes remain to be determined and compared. A new paradigm of the role of MMPs and their inhibitors in angiogenesis will be established.
In summary, the unexpected data demonstrates that MMPs and TIMPs may play a much more complex role in angiogenesis and tumor invasion and metastasis than that we have realized. The role and mechanisms of action of each MMP and each TIMP in angiogenesis are different depending on the tissue/cell specificity, the stages of endothelial differentiation, local microenvironmental factors, and tumorhost interactions. One possible scenario would be that, instead of blocking neovas-cularization, the MMP inhibitors may actually block angiostatin generation which, in turn, might cause unchecked and unlimited tumor growth and metastasis-the opposite of the desired effect7. Therefore, some of the clinical trials using synthetic MMP inhibitors may not be as successful as one might hope. Thus, more thorough and more mechanistic studies of potential roles of MMPs and their tissue and synthetic inhibitors in angiogenesis and tumor invasion and metastasis are still major tasks to be accomplished.
References
Birkedal-Hansen H . Proteolytic remodeling of extracellular matrix. Curr Opin Cell Biol 1995; 7:728–35.
Sang QA, Douglas DA . Computational Sequence Analysis of Matrix Metalloproteinases. J Protein Chem 1996; 15:137–60.
Chambers AF, Matrisian LM . Changing views of the role of matrix metalloproteinases in metas- tasis. J Natl Cancer Inst 1997; 89:1260–70.
Folkman J . Angiogenesis in cancer, vascular, rheumatoid and other disease. Nature Med 1995; 1:27–31.
Ray JM, Stetler Stevenson WG . The role of matrix metalloproteinases and their inhibitors in tumor invasion, metastasis and angiogenesis. Eur Respir J 1994; 7:2062–72.
Fisher C, Gilbertson Beadling S, Powers EA, Petzold G, Poorman R, Mitchell MA . Interstitial collagenase is required for angiogenesis in vitro. Dev Biol 1994; 162:499–510.
Moses MA . The regulation of neovascularization by matrix metalloproteinases and their inhibitors. Stem Cells 1997; 15:180–9.
Schnaper HW, Grant DS, Stetler Stevenson WG et al. Type IV collagenase(s) and TIMPs modulate endothelial cell morphogenesis in vitro. J Cell Physiol 1993; 156:235–46.
Unemori EN, Ferrara N, Bauer EA, Amento E . Vascular endothelial growth factorinduces in- terstitial collagenase expression in human endothelial cells. J Cell Physiol 1992; 153:557–62.
Zucker S, Conner C, DiMassmo BI et al. Thrombin induces the activation of progelatinase A in vascular endothelial cells, physiologic regulation of angiogenesis. J Biol Chem 1995; 270:23730–8.
Douglas DA, Shi YE, Sang QA . Computational sequence analysis of the tissue inhibitor of metalloproteinase family. Minireview. J Protein Chem 1997; 16:237–55.
Gomez DE, Alonso DF, Yoshiji H, Thorgeirsson UP . Tissue inhibitors ofmetalloproteinases: structure, regulation and biological functions. Eur J Cell Biol 1997; 74:111–22.
Johnson MD, Kim H RC, Chesler L, Tsao Wu G, Bouck N, Polverini PJ . Inhibition of angio- genesis by tissue inhibitor of metalloproteinase. J Cell Physiol 1994; 160:194–202.
Thorgeirsson UP, Yoshiji H, Sinha CC, Gomez DE . Breast cancer; tumor neovasculature and effect of tissue inhibitor of metalloproteinases 1 (TIMP-1) on angiogenesis. in vivo 1996; 10:137–44.
Murphy AN, Unsworth EJ, Stetler Stevenson WG . Tissue inhibitor of metalloproteinases 2 inhibits bFGF induced human microvascular endothelial cellproliferation. J Cell Physiol 1993; 157:351–8.
Anand Apte B, Pepper MS, Voest E et al. (1997) Inhibition of angiogenesis by tissue inhibitor of metalloproteinase 3. Invest. Ophthalmol Vis Sci 1997; 38:817–23.
Wang M, Liu YE, Greene J et al. Inhibition of tumor growth and metastasis of human breast cancer cells transfected with tissue inhibitor of metalloproteinase 4. Oncogene 1997; 14:2767–74.
O'Reilly MS, Holmgren L, Shing Y et al. Angiostatin: A novel angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. Cell 1994; 79:315–28.
Dong Z, Kumar R, Yang X, Fidler IJ . Macrophage derived metalloelastase is responsible for the generation of angiostatin in Lewis Lung Carcinoma. Cell 1997; 88:801–10.
Patterson BC, Sang QA, Angiostatin converting enzyme activities of human matrilysin (MMP-7) and gelatinase B/type IV collagenase (MMP-9). J Biol Chem 1997; 272:28823–5.
Acknowledgements
This work was in part supported by a Grant-in-Aid AHA 9601457 from the American Heart Association, Florida Affiliate (to Q. X. A. S.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sang, Q. Complex role of matrix metalloproteinases in angiogenesis. Cell Res 8, 171–177 (1998). https://doi.org/10.1038/cr.1998.17
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.1998.17
Keywords
This article is cited by
-
Angiogenic signaling pathways and anti-angiogenic therapy for cancer
Signal Transduction and Targeted Therapy (2023)
-
Angiogenic content of microparticles in patients with diabetes and coronary artery disease predicts networks of endothelial dysfunction
Cardiovascular Diabetology (2022)
-
Effects of metal nanoparticles on tight junction-associated proteins via HIF-1α/miR-29b/MMPs pathway in human epidermal keratinocytes
Particle and Fibre Toxicology (2021)
-
Skeleton-vasculature chain reaction: a novel insight into the mystery of homeostasis
Bone Research (2021)
-
Imatinib modulates pro-inflammatory microenvironment with angiostatic effects in experimental lung carcinogenesis
Inflammopharmacology (2020)